Cyclothymic Disorder (Cyclothymia): Symptoms, Diagnosis, and Management
Mood disorders exist on a vast and complex spectrum, ranging from the occasional “blues” to severe clinical crises. At the center of this spectrum lies cyclothymic disorder, a condition that is frequently misunderstood, underdiagnosed, and often dismissed as mere “moodiness.” However, for those living with it, cyclothymia represents a chronic challenge that requires significant emotional regulation and clinical support.
What Is Cyclothymic Disorder?
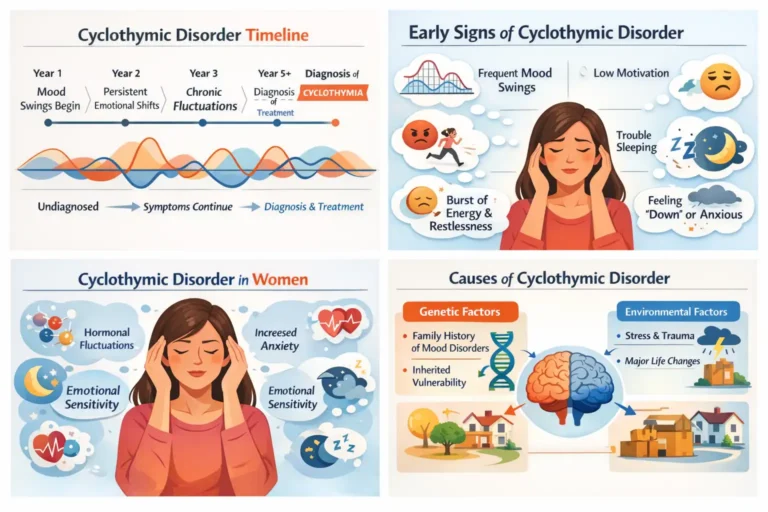
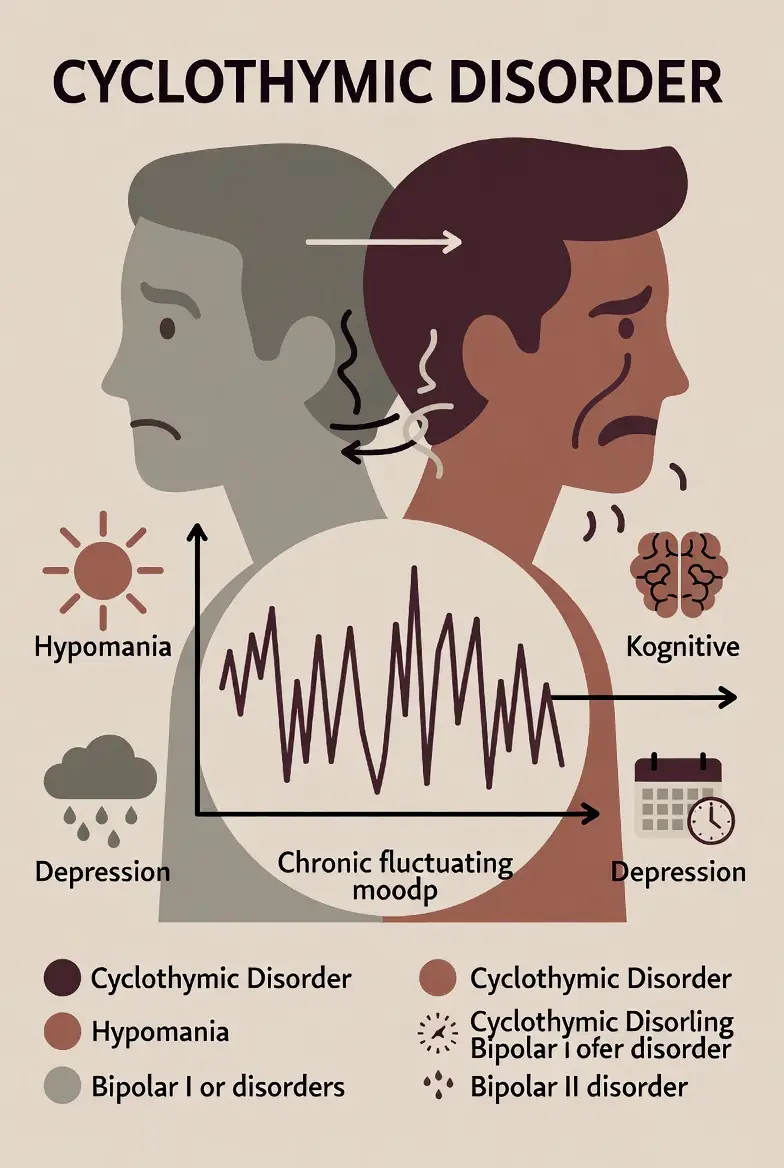
Cyclothymic disorder, often referred to simply as cyclothymia, is a chronic mood disorder characterized by numerous periods of hypomanic symptoms and periods of depressive symptoms. While these “highs” and “lows” are distinct, they do not meet the full severity or duration requirements for a major depressive episode or a manic episode.
In the field of psychology, cyclothymic disorder is classified as a milder, yet more chronic, form of bipolar disorder. Think of it as a “sub-threshold” version of its more famous relatives, Bipolar I and Bipolar II. Because the symptoms are less intense, individuals often avoid seeking help, assuming their fluctuating temperament is simply part of their personality. However, the constant “emotional rollercoaster” can significantly impair social, occupational, and personal functioning. Without intervention, cyclothymia can cause long-term strain on relationships and, in some cases, may even progress into a more severe bipolar diagnosis.
Common Misconceptions
Often, cyclothymia is dismissed as “just being moody” or having a “mercurial temperament.” However, the medical definition requires that these shifts cause significant distress or impairment in social, occupational, or other important areas of functioning. It is not a personality trait; it is a neurobiological condition where the brain’s “mood thermostat” is unable to maintain a steady temperature, leading to constant, exhausting recalibration.
Cyclothymic Disorder Symptoms: What Does It Look Like?
When asking what cyclothymic disorder looks like, the answer is found in the “in-between” spaces of emotion. The symptoms are divided into two distinct phases: hypomanic (the highs) and depressive (the lows).
Hypomanic Symptoms
During the “up” periods, an individual may feel significantly better than usual, but not to the point of losing touch with reality. Symptoms include:
- An exaggerated sense of happiness or well-being (euphoria).
- Extreme optimism and inflated self-esteem.
- Decreased need for sleep without feeling fatigued.
- Rapid speech and racing thoughts.
- Increased drive to perform or achieve goals (social, work, or sexual).
- High distractibility and physical agitation.
Depressive Symptoms
The “down” periods are characterized by a low mood that feels heavy but does not reach the debilitating depth of Major Depressive Disorder (MDD). Cyclothymia symptoms in this phase include:
- Feeling sad, hopeless, or empty.
- Irritability, especially in children and adolescents.
- Loss of interest in activities once enjoyed.
- Changes in weight or appetite.
- Feelings of worthlessness or excessive guilt.
- Fatigue or slowed movement.
- Difficulty concentrating or making decisions.
Cyclothymic Disorder in Women vs. Men
While the disorder affects both genders, research suggests that cyclothymic disorder in women may be diagnosed more frequently in clinical settings. Women may report more depressive symptoms and physical manifestations of the disorder, such as changes in appetite or sleep, whereas men may present with higher levels of irritability or impulsive “goal-directed” behavior during hypomanic phases.
How Long Does Cyclothymic Disorder Last?

Unlike a single episode of depression that might lift after a few months, cyclothymia is defined by its persistence. According to the DSM-5, for a diagnosis to be made in adults, these mood swings must be present for at least two years. For children and adolescents, the requirement is one year.
During this time, the symptomatic periods must be present at least half the time, and the individual must not be symptom-free for more than two months at a time. This chronic nature means that cyclothymic disorder episodes don’t necessarily have a clear start and end date; rather, the individual lives in a state of constant flux.
Causes & Triggers of Cyclothymic Disorder
The medical community is still investigating the exact causes of cyclothymic disorder, but it is generally accepted that a combination of factors is at play.
- Genetic Vulnerability: There is a strong hereditary link. People with cyclothymia are more likely to have family members with Bipolar I or Bipolar II, suggesting a shared genetic architecture.
- Neurobiology: Imbalances in brain chemicals (neurotransmitters) like serotonin, dopamine, and norepinephrine are believed to drive the mood cycles.
- Environmental Triggers: Traumatic life events, prolonged stress, or significant life changes can trigger the onset of symptoms.
- Sleep and Substance Use: Disruption of the circadian rhythm (sleep-wake cycle) is a major trigger for cyclothymic episodes. Additionally, the use of alcohol or drugs can exacerbate the “cycling” effect, often leading to a worsening of the disorder over time.
DSM-5 Diagnostic Criteria for Cyclothymic Disorder
The DSM-5 criteria are the gold standard for diagnosis. Professionals, such as those cited in StatPearls cyclothymic disorder literature, look for the following specific markers:
- Duration: Numerous periods of hypomanic symptoms and depressive symptoms for at least 2 years (1 year for youth).
- Frequency: Symptoms are present at least half the time, with no symptom-free period exceeding 2 months.
- Severity: Criteria for a major depressive, manic, or hypomanic episode have never been met.
- Exclusion: The symptoms are not better explained by schizoaffective disorder, schizophrenia, or other psychotic disorders.
- Substance/Medical Status: The symptoms are not attributable to a substance (e.g., drug abuse, medication) or another medical condition.
- Distress: The symptoms cause clinically significant distress or impairment in social, work, or other areas of functioning.
ICD-10 Classification & Coding
While the DSM-5-TR (Diagnostic and Statistical Manual of Mental Disorders) serves as the definitive diagnostic manual for clinicians in North America, the ICD-10 (International Classification of Diseases, 10th Revision) is the global standard for health management, clinical statistics, and insurance reimbursement. Within this international framework, Cyclothymic Disorder is classified under the “Mood (Affective) Disorders” section.
The Significance of Code F34.0
The official Cyclothymic disorder ICD-10 code is F34.0. This alphanumeric identifier is more than just a label for a medical chart; it is a critical tool that bridges the gap between clinical observation and institutional support.
- Validation of Medical Necessity: By assigning a specific code like F34.0, the World Health Organization (WHO) validates that cyclothymia is a distinct biological and psychological entity. This prevents it from being dismissed by insurance companies as a “general personality issue” or a non-clinical “lifestyle concern.”
- Standardization of Care: Whether a patient is in London, Tokyo, or New York, the F34.0 code ensures that the diagnosis remains consistent. This allows for international research, enabling scientists to track the prevalence of the disorder and the effectiveness of treatments across different populations.
Detailed ICD-10 Classification Breakdown
To understand where cyclothymia fits in the global medical landscape, one must look at the hierarchy of the “F” codes, which represent Mental and Behavioral Disorders. The ICD-10 organizes mood disorders based on the nature of the episodes and their persistence.
The F30–F39 Block: Mood (Affective) Disorders
- F30: Manic episode (Single episodes of mania).
- F31: Bipolar affective disorder (Cycling between mania and depression).
- F32: Depressive episode (Single episodes of depression).
- F33: Recurrent depressive disorder.
- F34: Persistent mood (affective) disorders. This is where cyclothymia resides because the symptoms are chronic and enduring rather than episodic.
- F34.0: Cyclothymic disorder.
- F34.1: Dysthymia (Chronic low-grade depression).
The placement of cyclothymia under F34 is significant because it highlights the persistence of the condition. Unlike episodic disorders, which may have long periods of total remission, F34 disorders are characterized by an ongoing, years-long struggle with mood regulation.
Transitioning to ICD-11
It is important to note that as of 2026, many health systems are in the middle of a multi-year transition to the ICD-11. In this newer version, the classification has become even more precise. In the ICD-11, Cyclothymic Disorder (Code 6A62) is placed firmly within the “Bipolar or Related Disorders” category. This shift is significant because it moves the disorder away from being a “persistent mood disorder” (ICD-10) and aligns it more closely with the biological “spectrum” of bipolarity.
Clinical and Insurance Relevance
For the patient, the ICD-10 classification is often the “key” that unlocks professional help:
- Reimbursement: Insurance providers require an ICD code to process claims for psychotherapy, psychiatric evaluations, and prescription medications. Without the F34.0 designation, many life-changing mood stabilizers would be prohibitively expensive.
- Diagnostic Specificity: Using the F34.0 code tells other healthcare providers that the patient has a specific biological sensitivity to mood-altering substances. This is vital when a GP or surgeon considers prescribing medications like steroids or certain stimulants, which can trigger a hypomanic swing in those with a cyclothymic profile.
- Electronic Health Records (EHR): Most modern hospitals use EHR systems that rely on ICD codes to trigger specific treatment protocols. A code of F34.0 helps ensure the patient isn’t incorrectly funneled into a “unipolar depression” treatment track, which could be harmful.
Cyclothymic Disorder vs. Other Bipolar Disorders
The most frequent question patients ask is: “How does cyclothymic disorder differ from bipolar?” or simply, “Is cyclothymic disorder bipolar?” While they exist on the same spectrum, they are distinct clinical diagnoses.
The Spectrum of Intensity
The primary difference lies in the intensity of the episodes.
- Bipolar I: Requires at least one full manic episode (often involving hospitalization or psychosis) and usually major depressive episodes.
- Bipolar II: Requires at least one hypomanic episode and at least one major depressive episode.
- Cyclothymia: Consists of hypomanic symptoms and depressive symptoms that never reach the full diagnostic threshold for a “Major Episode.”
Comparison Table: Cyclothymia vs. Bipolar 1 & 2
| Feature | Cyclothymic Disorder | Bipolar II Disorder | Bipolar I Disorder |
| High State | Hypomanic symptoms (Mild) | Full Hypomania (Moderate) | Full Mania (Severe) |
| Low State | Depressive symptoms (Mild) | Major Depression (Severe) | Major Depression (Severe) |
| Duration | 2 Years (Chronic) | Episodic | Episodic |
| Functioning | Distracted/Unstable | Severely impaired during lows | Often requires hospitalization during highs |
While cyclothymia is often called “Bipolar 3” in informal settings, it is unique because of its chronicity. A person with Bipolar I might have a manic episode and then months of stability. A person with cyclothymia rarely experiences more than eight weeks of a “level” mood, making the constant adaptation to shifting energy levels an exhausting daily reality.
Cyclothymia vs. Other Mood Disorders
Distinguishing cyclothymia from other disorders is a complex task for even seasoned clinicians. It is often confused with Persistent Depressive Disorder (PDD), formerly known as dysthymic disorder.
- Dysthymia/PDD: This involves a chronic low mood for at least two years. The key difference is that PDD does not include the “up” periods (hypomania). It is a flat line of low energy and sadness.
- Major Depressive Disorder (MDD): MDD is episodic and severe. Cyclothymia’s lows are more frequent but less deep than MDD.
- Borderline Personality Disorder (BPD): BPD also involves rapid mood swings, but these are usually triggered by interpersonal conflict or fear of abandonment. Cyclothymic swings are often more biological and can occur without a specific external event.
How Is Cyclothymic Disorder Diagnosed?
There is no “blood test” or single cyclothymic disorder test that can confirm a diagnosis. Instead, the process is longitudinal.
The Diagnostic Process
- Clinical Interview: A psychiatrist or psychologist will take a detailed history, looking for the 2-year pattern of mood shifts.
- Physical Exam: To rule out thyroid issues, hormonal imbalances, or vitamin deficiencies that can mimic mood swings.
- Mood Tracking: Patients are often asked to keep a “mood diary” for several weeks or months. This helps the clinician see the frequency of the “ups” and “downs.”
- Screening Tools: Tools like the Hypomania Check List (HCL-32) or the Mood Disorder Questionnaire (MDQ) may be used to identify sub-threshold symptoms.
The goal is to determine if the person’s mood is a reaction to life events or a persistent biological pattern. Because many people only seek help during the “low” periods, the “up” periods (which often feel productive and positive) are frequently missed, leading to a misdiagnosis of simple depression.
Treatment for Cyclothymic Disorder
The goal of cyclothymic disorder treatment is to “flatten the curve”—reducing the frequency and intensity of the swings to help the individual achieve emotional stability.
Psychotherapy
Therapy is the cornerstone of managing cyclothymia.
- Cognitive Behavioral Therapy (CBT): Focuses on identifying the “thought distortions” that occur during highs and lows. It teaches the patient to recognize the early signs of a mood shift.
- Interpersonal and Social Rhythm Therapy (IPSRT): This is highly effective for spectrum disorders. It focuses on stabilizing daily routines—eating, sleeping, and working at the same time every day—to help regulate the body’s internal clock.
- Dialectical Behavior Therapy (DBT): Useful for developing “distress tolerance” and emotional regulation skills.
Lifestyle Interventions
Because cyclothymia is sensitive to biological triggers, lifestyle changes are often as important as clinical treatment:
- Strict Sleep Hygiene: Going to bed and waking up at the same time every day is essential for mood stability.
- Avoiding Alcohol and Caffeine: These substances can “spike” or “crash” the nervous system, triggering an episode.
- Stress Management: Yoga, meditation, and regular exercise help buffer the nervous system against environmental stressors.
Medications for Cyclothymic Disorder
When lifestyle and therapy aren’t enough, cyclothymic disorder medication may be prescribed. The goal is mood stabilization rather than “fixing” a single state.
- Mood Stabilizers: Medications like Lithium or certain anticonvulsants (e.g., Lamotrigine, Valproate) are often the first line of defense. They help prevent the “poles” from becoming too extreme.
- Antipsychotics: In some cases, low-dose second-generation antipsychotics (e.g., Quetiapine) are used to help with sleep and irritability.
- The Antidepressant Caution: Doctors are often cautious about prescribing standard antidepressants (SSRIs) for cyclothymia. In some individuals, antidepressants can trigger a “switch” into a hypomanic state or cause rapid cycling, where the mood swings become even faster and more unstable.
Living With Cyclothymic Disorder
Learning how to deal with cyclothymic disorder is an ongoing process of self-discovery and boundary setting. Because the disorder is chronic, “management” is a more realistic goal than a “cure.”
Daily Coping Strategies
Individuals who thrive with cyclothymia often adopt a “scientist” mindset toward their own emotions. By using mood-tracking apps or journals, they can identify patterns. For example, a person might notice that their hypomanic periods always follow a week of high stress at work.
- The “Wait 48 Hours” Rule: During hypomanic symptoms, impulsivity is high. Many patients implement a rule to wait 48 hours before making any major purchases or life decisions to ensure the “high” isn’t driving the choice.
- Relationship Transparency: Cyclothymia can be hard on partners. Openly communicating that “I am feeling a bit low today, and it isn’t about you” can prevent the interpersonal friction that often accompanies mood shifts.
Workplace and Productivity
In professional settings, what cyclothymic disorder looks like can vary from being the “star employee” during a high to being seen as “unreliable” during a low. Successful professionals with cyclothymia often front-load their work during periods of high energy while maintaining a baseline of “survival tasks” for when their mood dips.
When Did Cyclothymic Disorder Become a Diagnosis?
The recognition of mild mood cycling dates back to the 19th century. German psychiatrist Karl Ludwig Kahlbaum first used the term “cyclothymia” in 1863 to describe what he saw as a temperament-based version of “circular insanity.”
- The Evolution of the Diagnosis: It wasn’t until the DSM-III in 1980 that cyclothymic disorder was formally recognized as a distinct psychiatric diagnosis rather than just a personality trait.
- Modern Understanding: Today, we view it through a “spectrum” lens. Instead of categorical boxes (you have it or you don’t), we see cyclothymia as part of a biological continuum of mood regulation.
Frequently Asked Questions
What are the diagnostic criteria for cyclothymic disorder?
According to the DSM-5, the criteria include: numerous periods of hypomanic and depressive symptoms for at least two years (one year in children); symptoms present at least half the time; never meeting the full criteria for a major depressive or manic episode; and significant distress or impairment in daily life.
How long do episodes last in cyclothymia?
Unlike Bipolar I, where a manic episode might last weeks, cyclothymic disorder episodes are often shorter and more frequent. A “high” or “low” might last just a few days, or it may linger for a week. The defining feature is not the length of a single episode, but the cumulative two-year pattern of cycling.
What triggers cyclothymic episodes?
Common triggers include disrupted sleep schedules, high-stress life events (both positive and negative), seasonal changes (reduced sunlight in winter), and the use of stimulants or alcohol. Hormonal fluctuations can also play a significant role.
What is the best medication for cyclothymia?
There is no single “best” medication, as treatment must be individualized. However, mood stabilizers like Lamotrigine or Lithium are frequently considered the first line of pharmacological defense. Low-dose atypical antipsychotics may also be used to manage specific symptoms like irritability or insomnia.
Is cyclothymic disorder a form of Bipolar?
Yes. In psychology, cyclothymic disorder is considered part of the bipolar spectrum. It is often referred to as a “milder” form of the illness, though the “milder” label refers to the intensity of the symptoms, not the impact on the person’s quality of life.
Conclusion
Living with cyclothymic disorder can feel like being at the mercy of an unpredictable tide. However, the science of 2026 has made it clearer than ever that stability is within reach. Through a combination of treatment for cyclothymic disorder—specifically mood-stabilizing medication and specialized therapies like CBT or IPSRT—individuals can find a middle ground.
Early recognition is the key. If you recognize these patterns in yourself or a loved one, seeking a professional evaluation is the first step toward reclaiming your emotional life. Cyclothymia is not a character flaw or a permanent “moody” personality; it is a biological condition that, once managed, allows for a life of great productivity, creativity, and balance.
Authoritative References
1. StatPearls (NCBI/National Library of Medicine)
2. Mayo Clinic –Cyclothymia Research Portal
3. American Psychiatric Association (APA) – Bipolar Disorders
4. Cleveland Clinic – Cyclothymia (Cyclothymic Disorder)
5. ICD-10 Data – F34.0 Diagnostic Code
Subscribe to Our Newsletter
Get mental health tips, updates, and resources delivered to your inbox.