Is Bipolar 1 or Bipolar 2 Worse? Differences, Symptoms, Severity, and Real-Life Impact

When a person is first diagnosed with a mood disorder, or when a family member is trying to understand a loved one’s struggle, one of the most immediate and frequent questions that arises is: Is bipolar 1 or 2 worse? This query is born out of a human need to quantify pain, predict the future, and understand the level of “seriousness” attached to a medical label.
However, in the world of psychiatry, the term “worse” is a complicated metric. Historically, clinical settings often viewed Bipolar I as the “classic” and more severe form of the illness due to the spectacular and often dangerous nature of full-blown mania. Conversely, Bipolar II was occasionally mischaracterized as “bipolar lite.” In 2026, our understanding has evolved. We now know that while the types differ in their diagnostic peaks, the “severity” of the condition is often measured by the depth of the valleys and the persistence of the symptoms.
Whether you are asking which is worse, bipolar 1 or 2, because you are struggling with a diagnosis or simply seeking to differentiate bipolar 1 and 2, this guide will explore the nuances of clinical severity versus the lived experience of suffering.
Bipolar I and Bipolar II Explained
To understand which of the two bipolar disorders is worse, 1 or 2, we must first define the landscape of the disorder. Bipolar disorder is a brain-based health condition that causes unusual shifts in mood, energy, activity levels, and the ability to carry out day-to-day tasks.
What Bipolar Disorder Is
At its core, bipolar disorder involves “episodes” that range from the extremes of high, energized behavior (mania or hypomania) to very low, sad, or hopeless periods (depression). The term manic depression vs bipolar is often discussed in clinical circles; while “manic depression” was the standard term for decades, it was replaced in the DSM (Diagnostic and Statistical Manual of Mental Disorders) to move away from the stigma and better reflect the biological nature of the “two poles” of the illness.
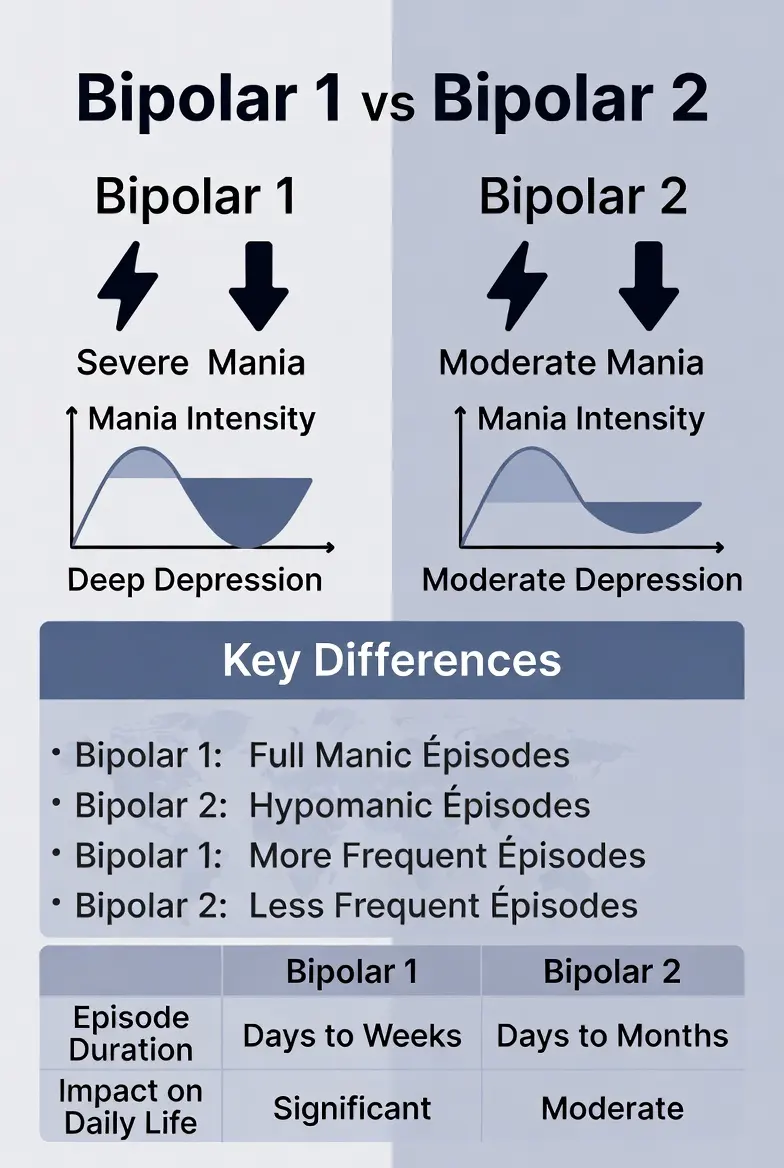
Bipolar I vs Bipolar II
- Bipolar I Disorder: Defined by the occurrence of at least one manic episode. While most people with Bipolar I also suffer from depression, it is not technically required for the diagnosis.
- Bipolar II Disorder: Defined by a pattern of depressive episodes and hypomanic episodes. Crucially, a person with Bipolar II has never had a full manic episode.
When people ask how serious Bipolar 2 is, they are often surprised to learn that it is a distinct clinical entity, not just a “milder version” of Type I. The two types are separated primarily by the “height” of the high episodes, but the impact on a person’s life can be equally devastating in both directions.
Mania (Bipolar I) vs Hypomania (Bipolar II)
The pivot point in the bipolar 1 vs 2 difference lies in the intensity of the “up” periods. This is where the distinction between mania vs hypomania becomes critical for diagnosis and safety.
Understanding Mania (Bipolar I)
In Bipolar I, the high is called mania. A manic episode is a distinct period of abnormally and persistently elevated, expansive, or irritable mood and increased energy lasting at least one week.
- Psychosis: Mania often includes psychotic features, such as delusions (believing things that aren’t true) or hallucinations (seeing or hearing things that aren’t there).
- Hospitalization: Because mania often results in severe impairment—such as spending life savings in a day or engaging in life-threatening behavior—hospitalization is frequently required to keep the person safe.
- Loss of Insight: A person in a manic state often has no idea they are ill, which makes bipolar mania symptoms particularly dangerous.
Understanding Hypomania (Bipolar II)
In Bipolar II, the high is called hypomania. The difference between bipolar and hypomania is largely one of degree and duration. Hypomania lasts at least four days and is a noticeable change from the person’s non-depressed self.
- Functionality: While the person may be unusually productive, talkative, or energetic, hypomania does not cause the severe social or occupational impairment seen in mania.
- No Psychosis: By definition, if there is psychosis, the episode is classified as mania, and the diagnosis becomes Bipolar I.
- Subtlety: Many people with Bipolar II initially enjoy hypomania, as it feels like a period of high confidence and creativity, which often leads to a delay in seeking help.
To truly differentiate bipolar 1 and 2, we must look beyond the “highs” and evaluate the entire clinical picture through the lens of the DSM-5 criteria.
i. Mood Episode Types and Frequency
In bipolar 1 and 2, the frequency of shifts can vary wildly. However, Bipolar I is often characterized by longer “level” periods between intense, shorter manic bursts. Bipolar II is frequently characterized by “rapid cycling” or lingering, low-grade depression that is punctuated by short bursts of hypomania.
ii. Severity Thresholds and Functioning
The bipolar 1 vs 2 disorder comparison often centers on functional impairment.
- Bipolar I is traditionally viewed as “worse” in an acute crisis. The risk of legal trouble, job loss from a single week of mania, and physical danger is extremely high.
- Bipolar II is often “worse” in terms of chronic disability. Studies show that people with Bipolar II spend significantly more time in the depressive phase than those with Bipolar I. This chronic, “smoldering” depression can lead to long-term erosion of relationships and career stability.
iii. Diagnostic Transitions
A key rule in psychiatry is that the diagnosis moves upward, but never downward. If a person diagnosed with Bipolar II experiences just one single manic episode or one psychotic break during a high, their diagnosis is permanently changed to Bipolar I. You cannot “go back” to being Bipolar II, as the presence of mania indicates a different underlying neurological vulnerability.
iv. Manic vs. Hypomanic Symptoms
While both types involve “elevated mood,” the expression differs:
- Bipolar 1 Symptoms (Mania): Extreme grandiosity, decreased need for sleep (sometimes 0 hours for days), racing thoughts that become incoherent (flight of ideas), and high-risk investments or sexual encounters.
- Bipolar 2 Symptoms (Hypomania): Increased “goal-directed” activity, being unusually “chatty” or witty, decreased need for sleep (3-4 hours), and a sense of being “on top of the world” without losing touch with reality.
v. The Depression Comparison
Interestingly, when people ask which bipolar disorder is worse, 1 or 2, they often overlook the “lows.”
- In Bipolar I, depression is often profound and paralyzing.
- In Bipolar II, the depression is not just profound; it is often more frequent and longer-lasting. Because the “highs” of Bipolar II are less extreme, the “lows” feel even heavier and more permanent. The suicide attempt rate in Bipolar II is equal to, and in some studies higher than, that of Bipolar I, largely due to the relentless nature of the depressive episodes.
Mixed Features
Both types can experience “mixed features,” where the energy of mania/hypomania meets the dark mood of depression. This is often described as the most dangerous state in all of psychiatry, as the person has the “energy” to act on the “hopelessness” of their depression.
For a quick reference to see which is more serious, bipolar 1 or Bipolar 2, use the following comparison chart.
| Feature | Bipolar I Disorder | Bipolar II Disorder |
| Highest Mood Peak | Full Mania (Severe) | Hypomania (Moderate) |
| Duration of High | 1 Week or more | 4 Days or more |
| Psychosis Risk | High (Common in Mania) | None (By Definition) |
| Hospitalization | Often Required | Rarely Required for Highs |
| Depression Type | Severe / Major | Severe / Major (Often Chronic) |
| Functionality during “High” | Severely Impaired | Often High-Functioning |
| Suicide Risk | Very High | Very High (due to depression) |
| Primary Challenge | Acute Crisis / Safety | Chronic Depression / Stability |
So… Which Is Worse: Bipolar 1 or Bipolar 2?
When directly addressing the question of which is worse, bipolar 1 or 2, the answer depends entirely on whether you are looking through a clinical lens or a personal, day-to-day lens. There is a common misconception that Type 2 is a “milder” version, but the reality is more nuanced.
Clinically “More Severe”: Bipolar I
From a medical standpoint, Bipolar I is often considered more “serious” because of the acute danger of mania. A person in a manic state can destroy their entire life—financially, legally, and socially—in a matter of days. The risk of psychosis and the frequent need for involuntary hospitalization make Bipolar I a high-intensity clinical emergency. If “worse” means “most likely to result in a 911 call,” then Bipolar I takes the lead.
Harder to Live With: Bipolar II
If you define “worse” by the total number of days spent suffering, Bipolar II often carries a heavier burden. Because the hypomania of Type 2 is shorter and less disruptive, people with this diagnosis spend a much larger percentage of their lives in a state of debilitating bipolar depression.
- The “Invisible” Illness: Because Bipolar II lacks the dramatic “spectacle” of mania, friends and family may not realize how sick the person is, leading to a lack of support.
- The Suicide Gap: Statistically, the suicide risk in Bipolar II is staggering. The chronic nature of the depression, combined with the “agitated” energy of hypomania, can create a lethal combination of hopelessness and impulsivity.
Which Bipolar Disorder Is More Serious Medically?
When doctors evaluate which is more serious, bipolar 1 or Bipolar 2, they look at long-term disability and physical health.
- Emergency Risk: Bipolar I carries a higher risk of immediate physical harm due to the reckless nature of mania.
- Long-Term Disability: Bipolar II often results in higher rates of long-term disability claims because the chronic depression is so resistant to standard treatments.
- Comorbidities: Both types carry a high risk of “co-occurring” conditions. Substance use disorders are rampant in both cases as people attempt to “self-medicate.” However, Bipolar II is frequently seen alongside intense anxiety disorders and eating disorders, which complicates the treatment path.
Is Bipolar 1 or Bipolar 2 Harder to Live With?
While Bipolar I involves more intense “crises,” Bipolar II involves more intense “attrition.” When asking if bipolar 1 or 2 is harder to live with, many patients point to the following factors:
a. Daily Functioning and Reliability
In Bipolar I, the episodes are often “episodic”—meaning they have a clear beginning, middle, and end, with periods of relative stability in between. In Bipolar II, the mood shifts can be more “flickering.” A person might feel okay in the morning, hypomanic by lunch, and deeply depressed by dinner. This unpredictability makes maintaining a traditional 9-to-5 job or a long-term marriage exceptionally difficult.
b. Misdiagnosis and the Wait for Help
The average time it takes for a person with Bipolar II to get a correct diagnosis is over 10 years. They are often misdiagnosed with “Unipolar Depression” (standard depression) because they don’t recognize their hypomania as a symptom. Taking standard antidepressants without a mood stabilizer can actually make Bipolar II worse, causing rapid cycling or increased irritability.
Aggression, Anger, and Risk Behaviors

A common and stigmatizing question is: Which bipolar disorder is aggressive? It is important to clarify that aggression is not a diagnostic requirement for either type, but “irritable mania” is a real phenomenon.
Mania and Impulsivity
In Bipolar I, aggression is usually a byproduct of frustration or paranoia during a manic episode. If a manic person is told “no” or is prevented from carrying out a “grand plan,” they may become highly agitated.
Hypomania and Irritability
In Bipolar II, the “high” isn’t always happy. It often manifests as “dysphoric hypomania”—a state of being “revved up” but incredibly angry, impatient, and snappy. This “bipolar rage” can be just as damaging to relationships as the full-blown mania of Type I, even if it doesn’t lead to a police intervention.
Bipolar 1 vs 2 vs Cyclothymia
To understand the full spectrum, we must look at bipolar 1 vs 2 vs cyclothymia. If Bipolar I and II are the “major” versions of the disorder, Cyclothymic Disorder is the “chronic” version.
- Cyclothymia: Characterized by at least two years of many periods of hypomanic symptoms and many periods of depressive symptoms. However, the symptoms never meet the full criteria for a Major Depressive Episode or a Hypomanic Episode.
- The Spectrum: Think of it as a wave. Bipolar I has the highest peaks and lowest valleys. Bipolar II has moderate peaks and the lowest valleys. Cyclothymia is a constant, smaller “choppy” wave that never quite levels out but never quite hits the “tsunami” level of the others.
Do I Have Bipolar 1 or Bipolar 2?
Determining whether I have bipolar 1 or 2 is a process that must be conducted by a psychiatrist or a clinical psychologist. However, reflecting on your history can help you provide the most accurate information during an evaluation. Often, people seek a diagnosis after a “crash” into depression, forgetting or dismissing the “up” periods that occurred months or years prior.
Common Signs to Monitor
- The “Sleep” Test: If you went three days without sleep and felt “better than ever” or were highly productive, that points toward Bipolar I or II. If you were hallucinating or felt like you had supernatural powers during that time, it leans toward Bipolar I.
- The “Impact” Test: Did your high periods lead to an arrest, a divorce, or a stay in a psychiatric ward? That is a hallmark of Bipolar I mania. If your highs just made you a “workaholic” or very social, but your lows lasted for months, that suggests Bipolar II.
- Family History: Bipolar disorder has a strong genetic component. Knowing if a relative had “classic” manic depression (Bipolar I) or chronic depression with “moody” streaks (Bipolar II) can provide clinical clues.
Professional diagnosis is vital because bipolar 1 and 2 require different medication strategies. Misdiagnosing Bipolar II as simple depression can lead to the prescription of SSRIs, which may trigger “rapid cycling” or even flip a person into their first full manic episode.
Bipolar 1 vs Schizophrenia
Because Bipolar I involves psychosis during mania, it is frequently confused with other conditions. The bipolar 1 vs schizophrenia comparison is one of the most common diagnostic hurdles in psychiatry.
Psychosis Timing
The main differentiator is when the psychosis happens.
- Bipolar I: Psychosis occurs only within the context of a mood episode (extreme mania or extreme depression). When the mood is stable, the psychosis disappears.
- Schizophrenia: Psychosis can occur without any mood symptoms present. It is the primary feature of the illness, rather than a symptom of a “high” or a “low.”
Treatment Focus
While both may use “atypical antipsychotics,” Bipolar I treatment focuses on mood stabilization (preventing the wave), whereas schizophrenia treatment focuses primarily on managing the hallucinations and delusions themselves.
What Reddit Gets Right (and Wrong) About Bipolar 1 vs 2
If you search for bipolar 1 or 2 on Reddit, you will find thousands of threads where patients debate their suffering. These communities provide a unique “on the ground” perspective that clinical textbooks often miss.
What the Community Gets Right
Reddit users often highlight the “loneliness” of Bipolar II. The community frequently points out that because Bipolar II looks “normal” to the outside world, patients are often accused of “faking it” or “just being dramatic.” On the other hand, Bipolar I users often discuss the “shame” and “cleanup” required after a manic episode—losing friends, jobs, and dignity in a very public way.
Common Misconceptions
A common error on social platforms is the idea that Bipolar II can be managed with “willpower” or “just therapy” because it doesn’t involve “scary” mania. The community correctly pushes back against this, emphasizing that the depression in Bipolar II is biologically driven and requires the same medical rigor as Bipolar I.
Frequently Asked Questions
What is worse, bipolar 1 or 2?
There is no “better” or “worse” in terms of human suffering. Bipolar I is medically more acute (higher risk of emergency and psychosis), while Bipolar II is often more chronic (more time spent in debilitating depression). Both carry a high risk of suicide and require lifelong management.
Is Bipolar 2 less serious than Bipolar 1?
No. Bipolar 2 is just as serious. While the “highs” (hypomania) are less dangerous than the mania of Bipolar 1, the “lows” (depression) are often more frequent, longer-lasting, and harder to treat.
Can Bipolar 2 become Bipolar 1?
Yes. If a person with Bipolar 2 experiences just one single manic episode (lasting 7 days or requiring hospitalization) or one psychotic break, their diagnosis is officially changed to Bipolar 1.
Which bipolar disorder is more likely to cause hospitalization?
Bipolar 1 is much more likely to cause hospitalization during a manic episode because the person loses insight and may become a danger to themselves or others. Bipolar 2 is more likely to cause hospitalization for suicidal ideation during a depressive episode.
Is there a Bipolar 3?
While not an official DSM-5 diagnosis, some clinicians use “Bipolar 3” to describe “cyclothymia” or “medication-induced bipolar,” where a person only has manic-like symptoms when taking certain drugs or antidepressants.
Conclusion
Ultimately, the debate over whether bipolar 1 or 2 is worse is a distraction from the real goal: stability. Every individual’s brain chemistry is unique. One person with Bipolar I may have a single manic episode every ten years and live a highly functional life, while another person with Bipolar II may struggle daily with “rapid cycling” that prevents them from ever holding a steady job.
The severity of your illness is defined by how much it interferes with your ability to love, work, and stay safe. Whether you are dealing with the “fire” of Bipolar I mania or the “ice” of Bipolar II depression, both conditions deserve the highest level of medical care, empathy, and respect.
Authoritative References
1. American Psychiatric Association (APA): Bipolar Disorders
2. National Institute of Mental Health (NIMH): Bipolar Disorder
3. Mayo Clinic: Bipolar Disorder Diagnosis and Treatment
4. National Alliance on Mental Illness (NAMI): Bipolar Disorder
5. The Lancet Psychiatry: Bipolar Disorder Spectrum Research
Subscribe to Our Newsletter
Get mental health tips, updates, and resources delivered to your inbox.