What are the 7 types of bipolar disorder? Types, Symptoms, Causes, and Daily Life

To define bipolar disorder accurately, we must look at it as a chronic mood dysregulation condition. In psychology and medicine, it is recognized as a complex brain disorder that causes unusual, often extreme shifts in a person’s mood, energy, activity levels, and concentration.
When people ask what are the 7 types of bipolar disorder, clinicians typically refer to a spectrum that includes Bipolar I disorder, Bipolar II disorder, cyclothymic disorder, bipolar disorder with mixed features, bipolar disorder with rapid cycling, substance- or medication-induced bipolar disorder, and bipolar disorder due to another medical condition—each defined by distinct patterns of manic, hypomanic, and depressive episodes.
According to the DSM-5 definition of bipolar disorder (Diagnostic and Statistical Manual of Mental Disorders, 5th Edition), the condition is primarily characterized by the occurrence of at least one manic or hypomanic episode. Unlike standard “moodiness,” these episodes represent a distinct departure from a person’s typical behavior and are sustained over days or weeks.
The bipolar disorder medical definition emphasizes that this is a biological condition. It is not a character flaw or a temporary reaction to stress, but a physiological malfunction in the brain’s ability to maintain “emotional homeostasis.”
When you see the terms bipolar mood disorder meaning or bipolar affective disorder definition, they are referring to the same core illness. The word “affective” is simply a clinical term for “mood.”
Essentially, “bipolar” means “two poles.” These poles represent the two extremes of human emotion:
- The High Pole (Mania/Hypomania): A state of abnormally elevated energy, euphoria, or irritability.
- The Low Pole (Depression): A state of intense sadness, hopelessness, and low energy.
Bipolar Disorder Fact Sheet (Quick Overview)
If you are looking for a quick bipolar disorder fact sheet, here are the essential statistics and clinical realities as of 2026:
- Prevalence: Approximately 2.8% of the U.S. adult population is diagnosed with bipolar disorder annually.
- Age of Onset: The average age for symptoms to begin is 25, although it can manifest in teens or, more rarely, in children and older adults.
- The Gender Split: Bipolar disorder affects men and women almost equally, though the way it manifests (types and cycling frequency) often differs by sex.
- Nature of the Illness: It is a chronic, lifelong condition. While it cannot be “cured” in the traditional sense, it can be managed so effectively that many individuals remain symptom-free for years.
- Risk Factors: Genetics play a massive role; if a first-degree relative has the condition, your risk increases significantly.
Why Is Bipolar Disorder Also Called Manic-Depressive Illness?
Many people still use the terms bipolar disorder, manic depressive illness, or manic depression interchangeably. Historically, “manic depression” was the standard medical term for nearly a century.
The name was changed in the 1980s for two primary reasons:
- Clinical Accuracy: The term “bipolar” more accurately describes the “two-pole” nature of the illness and includes those who experience “hypomania” (a milder high), who didn’t quite fit the old “manic” label.
- Stigma Reduction: The word “manic” had become a pejorative in popular culture, often associated with “madness.” Using “bipolar disorder” helped frame the condition as a medical neurological issue rather than a behavioral one.
How Many Types of Bipolar Disorder Are There? (3, 4, 5, or 7?)
If you search the internet, you will find conflicting information. Some sources mention 3 types of bipolar disorder, while others claim there are five types of bipolar disorder or even 7 types of bipolar disorder. This confusion exists because of how the medical community classifies “specifiers” versus “types.”
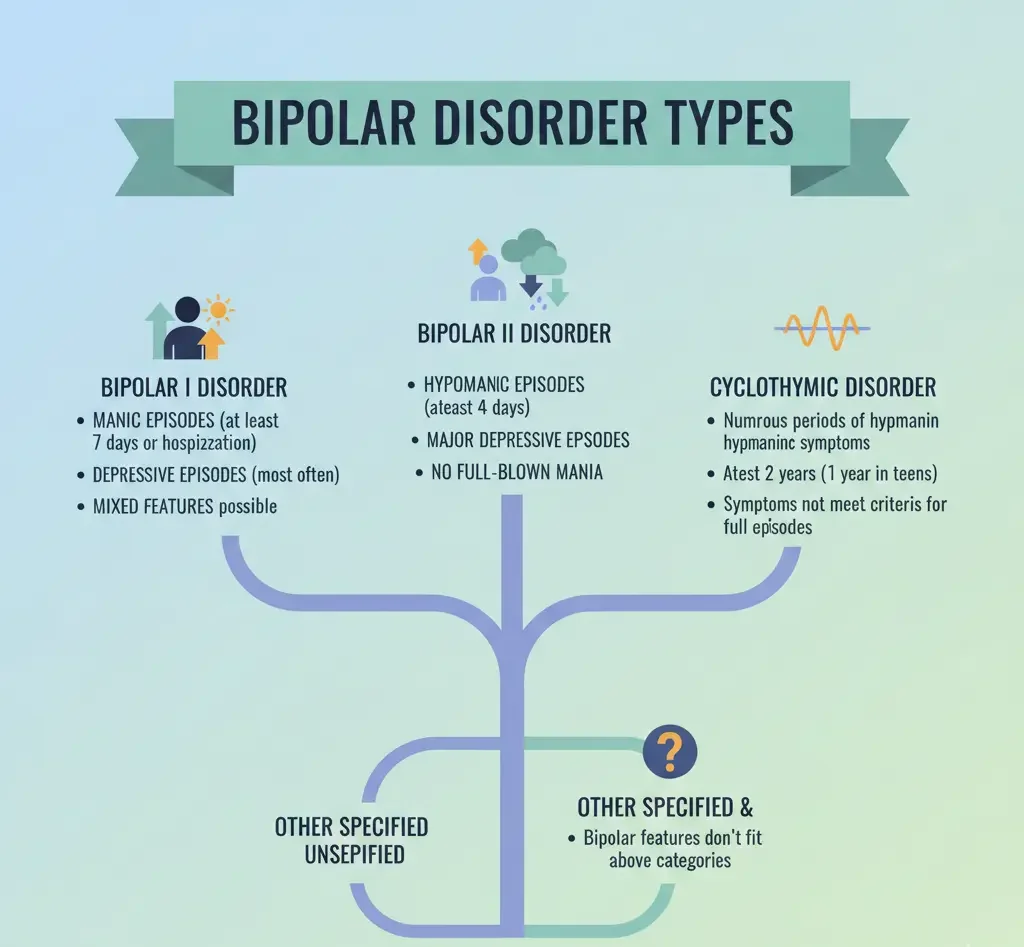
The Core DSM-5 Bipolar Types
Clinically, the DSM-5 recognizes three primary types:
- Bipolar I Disorder: Defined by manic episodes that last at least 7 days or are so severe they require hospitalization.
- Bipolar II Disorder: Defined by a pattern of depressive episodes and hypomanic episodes (but never full-blown mania).
- Cyclothymic Disorder (Cyclothymia): A milder form where mood swings are frequent but do not meet the full clinical criteria for a major manic or depressive episode.
Expanded Lists (Why Some Sources Say 5 or 7 Types)
The reason you see “7 types” mentioned in SEO searches and blogs is that modern psychiatry often breaks down the condition by its presentation or origin:
- Bipolar with Mixed Features: Feeling high energy and deep depression simultaneously.
- Rapid Cycling Bipolar: Experiencing four or more mood episodes in a 12-month period.
- Substance/Medication-Induced Bipolar: Mood swings triggered by drugs, alcohol, or certain medications.
- Other Specified/Unspecified Bipolar: Where symptoms don’t perfectly fit types 1, 2, or 3 but are clearly bipolar in nature.
The 7 Types of Bipolar Disorder Explained
To satisfy the modern clinical and educational understanding, let’s break down the 7 types of bipolar disorder as they are often categorized in specialized treatment centers.
1. Bipolar I Disorder
Bipolar I is defined by the presence of at least one Manic Episode. While depression often occurs, it is not actually a requirement for a Bipolar I diagnosis—the “high” is the defining marker.
The Risk of Psychosis: Bipolar I can involve a break from reality. This includes hallucinations (seeing or hearing things) or delusions. Because of the high risk of dangerous behaviors—like spending life savings or reckless driving—hospitalization is often necessary to keep the individual safe.
The Nature of Mania: This isn’t just a “good mood.” It is a distinct period of abnormally elevated or irritable mood and energy lasting at least one week. In this state, the brain’s “brakes” fail.
The “Superpower” Delusion: During mania, a person may experience Grandiosity. They might believe they have special connections to celebrities, undiscovered scientific insights, or even divine powers.
Total Loss of Sleep: A hallmark of Bipolar I is a “decreased need for sleep.” Unlike an insomniac who wants to sleep but can’t, a person in Bipolar I may stay awake for 4 or 5 days straight and feel completely refreshed and energetic.
2. Bipolar II Disorder
Bipolar II is frequently misunderstood as a “milder” version of the disorder. In reality, while the “highs” are less explosive, the “lows” are often more frequent and harder to treat.
The Hypomanic High: Energy Without the “Break”
The defining feature of Bipolar II is hypomania. Think of it as “mania-lite.” You are revving high, but you haven’t lost your grip on reality.
- The Experience: You may feel an “electric” sense of confidence. Your thoughts move faster, and you have a seemingly endless supply of energy. Unlike Bipolar I, you do not experience psychosis or require hospitalization during these phases.
- The Social Trap: Because hypomania often looks like high productivity, it is frequently mistaken for a “streak of genius.” You might start three new business projects or become the life of the party, making it hard for others to see it as a “symptom.”
The Depressive Reality: Where the Time is Spent
In Bipolar II, depressive episodes are the dominant feature. Research shows that people with Bipolar II spend significantly more time in the “low” phase than those with Bipolar I.
- Severity of the Crash: The depression in Bipolar II is often “melancholic.” It brings a profound sense of lethargy and physical heaviness. Simple tasks like brushing your teeth can feel like climbing a mountain.
- The Duration: These episodes can last for months. Because the “highs” are less disruptive, Bipolar II is often misdiagnosed as standard Clinical Depression for years. However, treating it with antidepressants alone can trigger “rapid cycling,” making the condition worse.
The Danger of “Mixed States”
One of the most dangerous aspects of Bipolar II is the Mixed Episode. This is when the energy of hypomania meets the despair of depression simultaneously. You feel “tired but wired.” You have dark, suicidal thoughts, but you have the agitated energy to act on them. This is the period where clinical vigilance is most critical.
If you want to know details about bipolar ii, you can read our details guidelines of bipolar ii.
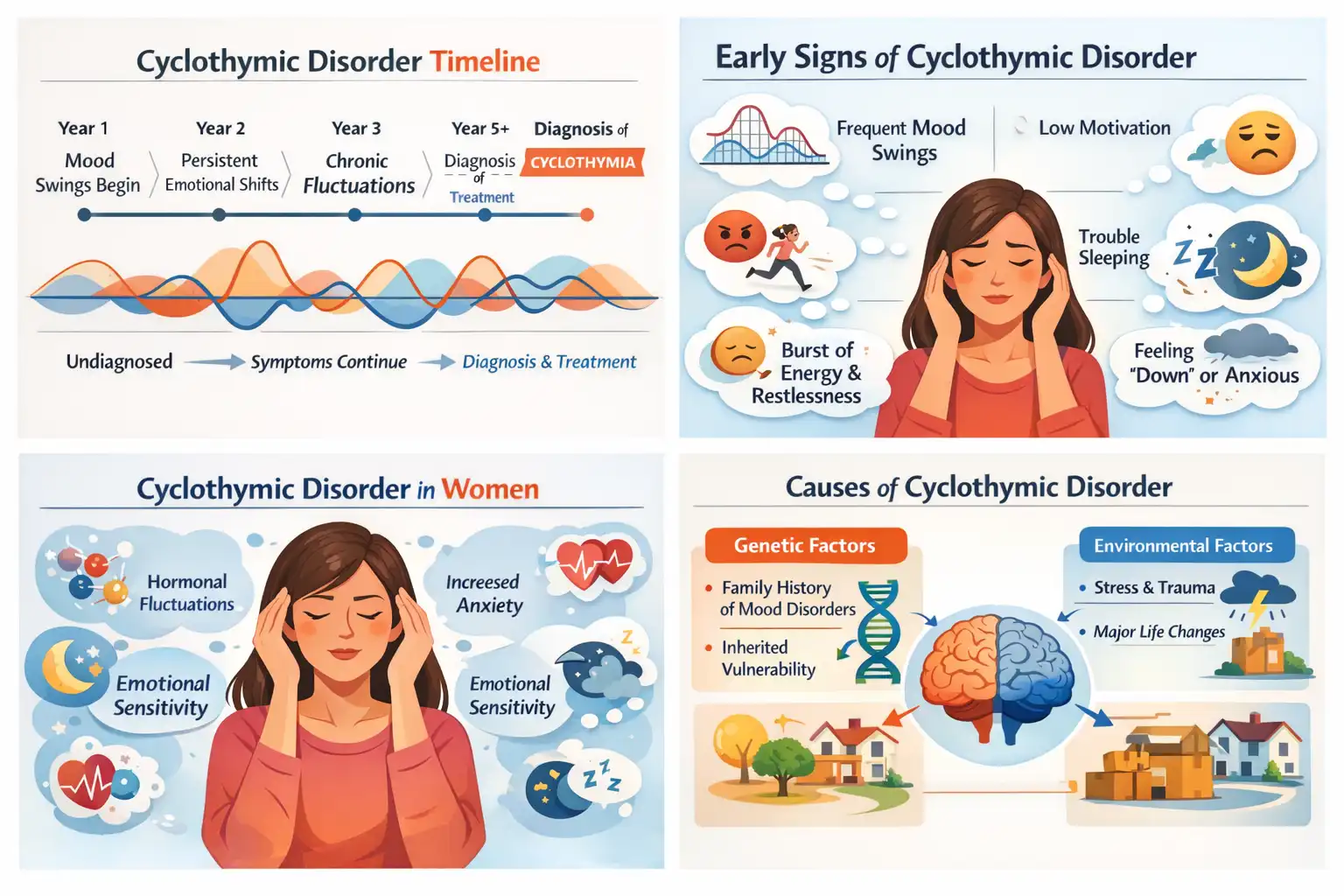
3. Cyclothymic Disorder: The Chronic Middle Ground
Cyclothymic disorder (or Cyclothymia) is often misunderstood as “personality quirks” or just being a “moody person.” However, it is a distinct clinical diagnosis within the Bipolar spectrum.
The Diagnostic Threshold
To meet the criteria, an adult must experience these fluctuating moods for at least two years (one year for children) without a break longer than two months. The hallmark of Cyclothymia is that the symptoms are sub-syndromal. This means:
- The “highs” are hypomanic but don’t quite meet the full criteria for a Hypomanic Episode.
- The “lows” are depressive but don’t reach the severity or duration of a Major Depressive Episode.
Living with the “Simmer”
Because the symptoms aren’t as “explosive” as Bipolar I, people with Cyclothymia often go undiagnosed for years. They may be viewed as hyper-productive and charismatic one week, and then irritable and withdrawn the next. However, because the cycle is chronic, it can be incredibly draining, often leading to difficulties in maintaining long-term relationships or steady employment.
4. Bipolar Disorder with Mixed Features: The “Tired and Wired” State
If Bipolar I is a pendulum swinging from left to right, “Mixed Features” (formerly known as a Mixed Episode) is what happens when the pendulum gets stuck in the middle while still vibrating at maximum speed. It is widely considered the most dangerous and uncomfortable state in psychiatry.
The Paradoxical Symptoms
In a mixed state, a person experiences the energy of mania and the agony of depression simultaneously. Common presentations include:
- Agitated Depression: Feeling a profound sense of hopelessness and “darkness,” but having the physical energy to pace the room for hours.
- Racing Thoughts of Despair: The mind is moving at 100 mph, but every thought is self-critical or suicidal.
- Pressure and Irritability: Unlike “pure” mania, which can be euphoric, mixed features are almost always dysphoric (unpleasant). There is a high level of skin-crawling agitation.
Clinical Risks
The reason clinicians take mixed features so seriously is the risk of suicide. In a standard major depressive episode, a person may feel suicidal but lack the energy to act on it (psychomotor retardation). In a mixed state, the person has the “manic energy” to carry out a plan.
5. Rapid Cycling: The High-Speed Specifier
“Rapid Cycling” is not a standalone diagnosis; rather, it is a specifier that clinicians add to a Bipolar I or II diagnosis. It describes a pattern where the “mood thermostat” is essentially broken, leading to frequent, exhausting shifts.
The “4 in 12” Rule
To be clinically defined as a rapid cycler, an individual must experience four or more distinct mood episodes (mania, hypomania, or depression) within a single 12-month period. These episodes must be separated by either a period of full remission or a “switch” to an episode of the opposite polarity.
Why Does It Happen?
While anyone can experience rapid cycling, research shows it is significantly more common in women. Two major “external” culprits often play a role:
- Thyroid Dysfunction: The endocrine system and mood are tightly linked. Hypothyroidism (an underactive thyroid) is frequently found in patients with rapid-cycling patterns.
- Antidepressant Use: For some with a latent bipolar vulnerability, taking an SSRI (like Prozac or Zoloft) without a mood stabilizer can “accelerate” the cycle, pushing the brain into a state of rapid flipping.
6. Substance/Medication-Induced Bipolar Disorder
This diagnosis is used when manic or depressive symptoms are a direct physiological consequence of a drug, toxin, or medication. It creates a “chicken or the egg” dilemma for doctors: is the drug causing the mood, or is the person using the drug to self-medicate a pre-existing mood disorder?
Common Triggers
- Stimulants: Cocaine and amphetamines (including some ADHD medications) can mimic full-blown mania, causing euphoria, insomnia, and grandiosity.
- Steroids: High doses of corticosteroids (like Prednisone) are notorious for causing “steroid psychosis” or manic-like irritability.
- Alcohol & Opioids: While often thought of as “downers,” the withdrawal phases from these substances can trigger profound depressive crashes or agitated manic states.
The “Trigger” Effect
The most critical aspect of Substance-Induced Bipolar is what happens after detox.
Unmasking: In other cases, the substance acts as a “key” that unlocks a genetic door. The drug triggers the first manic episode, but even after the drug is gone, the brain remains in a bipolar state, requiring lifelong management.
Resolution: In many cases, once the substance is out of the system for several weeks, the moods level out, and no further treatment is needed.
7. Other Specified and Unspecified Bipolar Disorder: The “In-Between” Reality
The DSM-5 (the manual used to diagnose mental health conditions) has very strict “gatekeeping” rules. For example, to be diagnosed with Bipolar II, a hypomanic episode must last at least four consecutive days. If a person experiences a textbook hypomanic “high” that only lasts two days but causes them to lose their job or ruin a relationship, they technically don’t qualify for Bipolar II.
This is where Other Specified and Unspecified diagnoses come in. They ensure that people who are suffering don’t fall through the cracks of medical bureaucracy.
Why “Other Specified” is Used
A clinician uses “Other Specified” when they want to communicate the exact reason why the patient doesn’t meet the standard criteria. Common examples include:
- Short-Duration Hypomania: The person has clear manic symptoms, but they only last 2–3 days instead of the required 4.
- Insufficient Symptoms: The person has a long duration of “highs,” but they only meet two of the required symptoms (e.g., racing thoughts and insomnia) instead of three or more.
- Bipolar II without Major Depression: A person experiences hypomania but has never hit the “rock bottom” of a major depressive episode.
The “Unspecified” Label
The “Unspecified” label is generally used in emergency situations or initial intakes. If a doctor sees a patient in a state of clear manic agitation but doesn’t have the patient’s full medical history or enough time to count the days of the episode, they use this label to ensure the patient receives mood-stabilizing treatment immediately while further observation takes place.
Bipolar I vs Bipolar II — What Is the Difference?
The most common question patients ask is: What Is the Difference Between Bipolar 1 and 2? The distinction is crucial because the treatment paths often differ.
| Feature | Bipolar I | Bipolar II |
| The “High” | Full Mania (may involve psychosis) | Hypomania (no psychosis) |
| Hospitalization | Often required during mania | Rarely required for the high |
| Depression | Common, but not required for diagnosis | Required for diagnosis; often severe |
| Functioning | Severely impaired during mania | Often “high-functioning” during hypomania |
Which Is the Worst Type of Bipolar Disorder?
Patients and families often ask, “which is the worst type of bipolar disorder?” Clinically, there is no “worst” type, as severity is subjective to the individual’s life circumstances.
- Bipolar I is often seen as more “dangerous” due to the risk of psychosis and legal/financial ruin during mania.
- Bipolar II and Mixed Features are often associated with a higher risk of self-harm and suicide because the depressive states are so frequent and intense.
- Rapid Cycling is considered the most “difficult to treat” because the brain is constantly in flux, making it hard for medications to “catch up.”
In truth, the “worst” type is simply the one that is currently untreated.
Signs and Symptoms of Bipolar Disorder
Identifying bipolar disorder requires a keen eye for patterns rather than isolated moods. While the “two poles” define the illness, the symptoms manifest in a wide range of behaviors that can look very different from person to person.
7 Signs of Bipolar Disorder (The Manic Phase)
In a manic or hypomanic state, the brain is essentially operating in “overdrive.” If you or a loved one are experiencing these 7 signs of bipolar disorder, it may indicate a manic episode:
- Decreased Need for Sleep: Feeling completely rested after only 2 or 3 hours of sleep, or sometimes no sleep at all, for several days.
- Pressured Speech: Talking much louder and faster than usual; it may feel impossible for others to interrupt.
- Racing Thoughts: A subjective feeling that thoughts are moving faster than they can be spoken, often jumping from one unrelated idea to another.
- Excessive Involvement in Risky Activities: Engaging in unrestrained buying sprees, sexual indiscretions, or foolish business investments.
- Inflated Self-Esteem or Grandiosity: Feeling “invincible” or possessing special powers or talents that don’t exist in reality.
- High Distractibility: The inability to filter out irrelevant external stimuli; the person is “pulled” toward every sound or movement in the room.
- Psychomotor Agitation: Physical restlessness, such as pacing or the inability to sit still for even a few minutes.
7 Signs of Bipolar Disorder (The Depressive Phase)
Conversely, the depressive pole is characterized by a “system shutdown.”
- Pervasive Sadness: Feeling empty, hopeless, or tearful most of the day, nearly every day.
- Anhedonia: A total loss of interest or pleasure in all, or almost all, activities that were once enjoyed.
- Significant Weight or Appetite Changes: Often losing weight without dieting or, in some cases, excessive overeating.
- Insomnia or Hypersomnia: Either the inability to sleep despite fatigue or sleeping for 12+ hours and still feeling exhausted.
- Psychomotor Retardation: Moving and speaking so slowly that it is observable by others (feeling like your limbs are made of lead).
- Feelings of Worthlessness: Excessive or inappropriate guilt, often over small mistakes from the past.
- Suicidal Ideation: Recurring thoughts of death or specific plans for self-harm.
Bipolar Disorder Symptoms in Females
While the core diagnostic criteria are the same, bipolar disorder symptoms in females often present unique challenges. Research in 2026 suggests that biological sex and hormones play a significant role in the illness’s trajectory.
- Hormonal Influence: Women often report that their mood cycles are exacerbated by their menstrual cycle, pregnancy, or menopause.
- Postpartum Vulnerability: Women with bipolar disorder have a significantly higher risk of developing postpartum psychosis or severe postpartum depression.
- Rapid Cycling: Women are statistically more likely than men to experience “rapid cycling,” where they flip between poles four or more times in a year.
- Misdiagnosis Risks: Women are frequently misdiagnosed with “Borderline Personality Disorder” or “Major Depressive Disorder” because their manic episodes may be less “grandiose” and more characterized by irritability and anxiety.
Signs of Bipolar Disorder — When Should You Take a Self-Test?
If you find yourself relating to the descriptions above, you might be wondering, “Could You Have Bipolar Disorder?” Taking a self-test can be a valuable first step in organizing your thoughts before speaking with a professional.
⚠️ Medical Disclaimer: A self-test is a screening tool, not a diagnostic instrument. A “high score” on a bipolar self-test does not mean you have the disorder; it simply means your symptoms warrant a clinical evaluation by a psychiatrist or psychologist.
Key Symptoms to Watch For
You should consider a professional evaluation if:
- Your mood swings are causing problems in your relationships or at work.
- Your “high” periods are followed by deep, debilitating “lows.”
- You have a family history of bipolar disorder or suicide.
- You have ever experienced psychosis (hallucinations or delusions) during a mood shift.
What Causes Bipolar Disorder?
There is no single cause of bipolar disorder. Instead, scientists view it through the “Biopsychosocial Model,” where multiple factors converge to trigger the illness.
Genetic Factors
Bipolar disorder is one of the most heritable mental health conditions. If you have an identical twin with the disorder, your risk is approximately 40% to 70%. Researchers have identified several clusters of genes responsible for how the brain regulates calcium signaling and neurotransmitter release.
Brain Chemistry and Structure
Advanced neuroimaging in 2026 shows that people with bipolar disorder often have:
- Neurotransmitter Imbalances: Fluctuations in dopamine (the reward chemical), serotonin (the mood chemical), and norepinephrine (the stress chemical).
- Structural Differences: A smaller or less active prefrontal cortex (the part of the brain that controls impulses) and an overactive amygdala (the brain’s emotional center).
Environmental Stressors
While genetics “prime” the brain, the environment often “pulls the trigger.” Severe trauma, childhood neglect, or prolonged periods of high stress can cause a latent genetic predisposition to manifest as a full-blown mood episode.
What Are the Triggers for Bipolar Disorder?

Even after a diagnosis is made and treatment has begun, certain factors can trigger a “breakthrough” episode. Identifying your personal triggers for bipolar disorder is essential for long-term stability.
- Sleep Deprivation: This is the #1 trigger for mania. Even one night of missed sleep can send a bipolar brain into a manic spin.
- High Stress: Major life events—both negative (job loss) and positive (getting married)—can trigger a shift.
- Substance Use: Alcohol and drugs (especially stimulants like cocaine or even excessive caffeine) interfere with the brain’s delicate chemical balance.
- Seasonal Changes: Many patients experience a “seasonal pattern,” often feeling manic in the bright light of spring and summer and depressed in the darkness of winter.
How to Handle a Bipolar Person (Supportive, Healthy Ways)
If you are a caregiver, learning how to handle a bipolar person requires a balance of empathy and firm boundaries.
During a Manic Episode
- Stay Calm: Do not get into an argument or try to “out-logic” someone in mania. Their brain is physically incapable of logical reasoning at that moment.
- Safety First: If they are engaging in dangerous behaviors (fast driving, excessive spending), try to gently steer them toward a safe environment or call their doctor.
- Minimize Stimuli: Turn down the lights, reduce noise, and keep conversations short and simple.
During a Depressive Episode
- Be Present: Sometimes simply sitting with them is more powerful than trying to “cheer them up.”
- Assist with Basics: Help them shower, eat a healthy meal, or take their medication. Depression makes small tasks feel like climbing Everest.
- Validate, Don’t Dismiss: Avoid saying things like “just snap out of it.” Instead, say, “I know you’re hurting, and I’m here for you.”
What Foods Should Bipolar People Avoid?
While diet cannot “cure” bipolar disorder, what you eat can significantly impact your medication’s effectiveness and your mood stability. What foods should bipolar people avoid?
- Excessive Caffeine: Found in coffee, energy drinks, and some sodas. Caffeine mimics mania by causing racing thoughts and heart palpitations.
- Alcohol: Alcohol is a central nervous system depressant. It can worsen the “lows” and interfere with almost every bipolar medication.
- High-Sugar Foods: Sugar causes “spikes and crashes” in energy levels, which can mimic or exacerbate mood cycling.
- Grapefruit Juice: This is a specific medical warning. Grapefruit juice can interfere with the metabolism of certain bipolar medications (like some antipsychotics and anticonvulsants), leading to dangerously high levels in the bloodstream.
Do People With Bipolar Disorder Live a Long Life?
When receiving a chronic diagnosis, one of the most pressing concerns is longevity. A common search query is, “Do people with bipolar live a long life?” The answer is multifaceted: while bipolar disorder is a serious condition that historically has been linked to a shorter lifespan, modern medicine and lifestyle interventions in 2026 have significantly narrowed that gap.
Life Expectancy Data
Statistically, individuals with bipolar disorder have historically seen a reduction in life expectancy of about 10 to 20 years. However, it is crucial to understand why this statistic exists. It is rarely the “mood swings” themselves that impact longevity, but rather the secondary effects of the illness:
- Cardiovascular Health: Chronic stress and certain older medications can increase the risk of heart disease and diabetes.
- Suicide Risk: Approximately 15% to 17% of those with bipolar disorder may succumb to suicide if the condition remains untreated.
- Lifestyle Factors: High rates of smoking and sedentary behavior during depressive episodes can impact long-term health.
Impact of Treatment on Longevity
The good news is that treatment changes everything. Research shows that individuals who are consistently treated with mood stabilizers like Lithium or modern atypical antipsychotics have a life expectancy nearly identical to the general population. Proper treatment reduces the physiological “wear and tear” on the brain and body caused by extreme cortisol spikes during mania and inflammation during depression.
What Disorders Were in Axis I? (DSM-IV Context)
For those looking back at their medical records or older psychology textbooks, the term “Axis I” frequently appears. Understanding what disorders were in Axis I helps clarify how the clinical view of bipolar disorder has evolved.
In the DSM-IV (the manual used until 2013), doctors used a “multiaxial” system to diagnose patients:
- Axis I: Clinical Disorders. This was the “main” diagnosis and included bipolar disorder, schizophrenia, major depressive disorder, and anxiety.
- Axis II: Personality Disorders and Intellectual Disabilities.
- Axis III: General Medical Conditions.
Why the Axis System Was Removed
The shift to the DSM-5 removed the axes entirely. The medical community realized that separating bipolar disorder (Axis I) from a person’s personality or physical health (Axis III) was a mistake. Bipolar disorder is not an “episodic guest” in the body; it is a permanent, biological reality that affects everything from heart rate to personality. Modern clinicians now use a single-axis, integrated approach that views the person as a whole.
How to Live Well with Bipolar Disorder (The Practical Path)
The H1 of this guide promises a look at how to live well, which is the “Practical/Lifestyle” core of the article. Managing bipolar disorder is 50% medication and 50% lifestyle “scaffolding.”
The Power of Routine and Structure
The bipolar brain is highly sensitive to disruptions in the “circadian rhythm”—the internal clock that regulates sleep, hunger, and energy. To live well, a person must become a “guardian of their routine.”
- Social Zeitgebers: These are external cues (like meal times or work schedules) that help keep your internal clock on track.
- Predictability: Going to bed and waking up at the same time every day—even on weekends—is the single most effective non-drug intervention for preventing mania.
Interpersonal and Social Rhythm Therapy (IPSRT)
In 2026, IPSRT has become a leading psychotherapy for bipolar disorder. It doesn’t just focus on “feelings”; it focuses on the timing of your life. By tracking your “Social Rhythm Metric,” you can see exactly when your routine starts to slip, allowing you to intervene before a full-blown episode begins.
Relationships and Social Support
Understanding how to handle a bipolar person isn’t just for caregivers; it’s for the individuals themselves as they navigate their social lives.
Communication During Stability
The best time to talk about bipolar disorder is when you are “euthymic” (stable). This is when you can create a “Wrap Plan” (Wellness Recovery Action Plan) with your partner or family.
- Identify Red Flags: “If you notice I’m starting to spend money impulsively, please remind me of our agreement to check in.”
- Crisis Contacts: Ensure your inner circle knows which doctor to call if you lose insight during a manic episode.
Setting Boundaries
Living well means knowing when to step back. If you are entering a depressive phase, it is okay to set boundaries on social obligations. Protecting your energy is a medical necessity, not a sign of selfishness.
Frequently Asked Questions (FAQ)
How many types of bipolar disorder are there really?
While the DSM-5 officially lists three (Bipolar I, Bipolar II, and Cyclothymic), most specialists recognize at least 7 types when including “Mixed Features,” “Rapid Cycling,” and “Substance-Induced” variations.
Is cyclothymic disorder a form of bipolar?
Yes. It is considered a milder, chronic form of the bipolar spectrum. While the highs and lows are less extreme, the “instability” can be just as disruptive to a person’s life if left unmanaged.
What is the most severe type of bipolar disorder?
Bipolar I is often considered the most “acute” due to the risk of psychosis and hospitalization. However, Bipolar II and Mixed States are often considered the most “burdening” because the depression can be more frequent and harder to treat.
Can bipolar disorder be managed long-term?
Absolutely. With the right combination of bipolar mood disorder medications, psychotherapy (like CBT or IPSRT), and strict sleep hygiene, many people live decades without a major episode.
What is the difference between manic and depressive episodes?
A manic episode is a “high-energy” state marked by decreased sleep and racing thoughts. A depressive episode is a “low-energy” state marked by sadness, lethargy, and a lack of interest in life.
Conclusion: Embracing a Balanced Life
Bipolar disorder is a formidable diagnosis, but it is not a life sentence. By understanding the definition of bipolar disorder as a physiological condition rather than a character flaw, you can begin to treat it with the same diligence as any other chronic illness.
Whether you are navigating Bipolar I vs Bipolar II, or searching for the 7 signs of bipolar disorder to help a loved one, remember that stability is built on the foundation of education, medication, and routine. With the tools available in 2026, living well with bipolar isn’t just a possibility—it is the new standard of care.
Authoritative References
Subscribe to Our Newsletter
Get mental health tips, updates, and resources delivered to your inbox.