What Causes Bipolar Disorder in the Brain? Biology, Triggers, and How Bipolar Works
For many individuals living with a diagnosis or watching a loved one struggle with mood swings, the most pressing question is often a search for “the why.” There is a deep-seated need to understand what causes bipolar disorder in the brain because, for a long time, mental health struggles were unfairly characterized as personal failings or lack of willpower.
When people search for these answers, they are often looking for validation. They want to know that the crushing weight of depression or the frenetic, uncontrollable energy of mania has a biological basis. Understanding the neuroscience behind the condition helps strip away the stigma, replacing shame with a medical framework for recovery. This article dives into the complex “machinery” of the bipolar brain, exploring how genetics, brain structure, and chemistry converge to create this unique neurobiological experience.
What Is Bipolar Disorder?
To understand the cause, we must first define the condition. Bipolar disorder is a chronic mental health condition characterized by significant fluctuations in mood, energy, and activity levels. Unlike the typical “ups and downs” most people experience, these shifts are intense, prolonged, and can interfere with a person’s ability to carry out day-to-day tasks.
Bipolar Meaning and Classification
The core of bipolar disorder lies in the “episodes.”
- Mania: A state of high energy, reduced need for sleep, and potentially risky behavior.
- Hypomania: A less severe version of mania found in Bipolar II.
- Depression: Intense sadness, hopelessness, and low energy.
It is important to distinguish between mood episodes and personality. Bipolar disorder is something a person has, not who they are. Between episodes, many people return to a stable “baseline” where their true personality shines through, unaffected by the biological “noise” of the disorder.
What Causes Bipolar Disorder in the Brain?
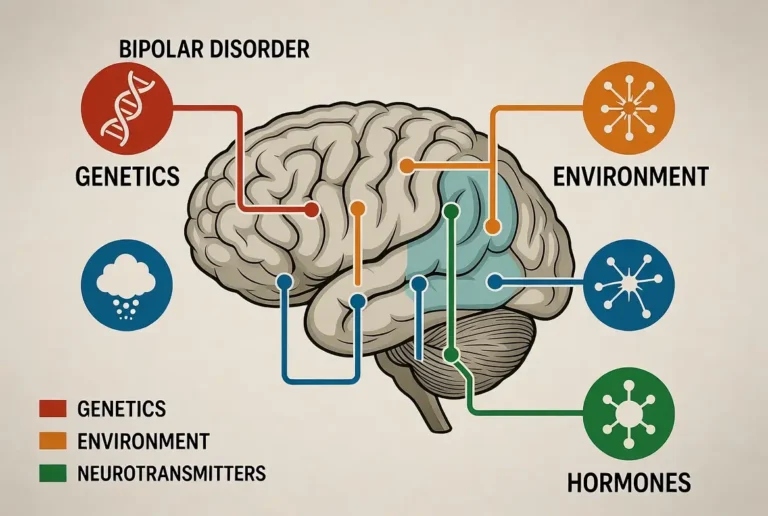
If you are looking for a “root cause,” science tells us there is no single “on-off switch” for bipolar disorder. Instead, what causes bipolar disorder in the brain is a combination of three primary factors:
- Biological Vulnerability: Differences in brain structure and the way brain cells communicate.
- Genetic Predisposition: Inherited traits that make the brain more sensitive to mood shifts.
- Environmental Triggers: External stressors that “activate” the underlying biological vulnerability.
Think of the brain like a highly sensitive thermostat. In a “normal” brain, the thermostat adjusts the temperature (mood) smoothly as the weather (life events) changes. In a bipolar brain, the thermostat is hypersensitive; a small draft might cause the furnace to blast (mania) or the cooling system to freeze (depression).
Bipolar Brain vs. Normal Brain: What’s Different?
Neuroimaging technology—like fMRI and PET scans—has allowed scientists to see the bipolar brain vs normal brain in real-time. These studies show that bipolar disorder isn’t just a “feeling”; it involves measurable physical differences in the brain’s architecture.
Emotional Regulation Networks
The biggest difference lies in how different parts of the brain talk to each other. In a typical brain, the prefrontal cortex (the “logical” part) acts as a brake on the limbic system (the “emotional” center).
In the bipolar brain, this connection is often weakened.
- Overactive Limbic System: The amygdala, which processes emotions like fear and joy, is often hyper-reactive in those with bipolar disorder.
- Underactive Prefrontal Cortex: During mood episodes, the prefrontal cortex may fail to provide the necessary “top-down” regulation to keep the limbic system in check. This leads to the intense, unchecked emotions characteristic of the disorder.
Neurotransmitters & Bipolar Disorder (Brain Chemistry Explained)
When people ask, “Which hormone causes bipolar disorder?” they are usually actually referring to neurotransmitters. While hormones (like cortisol or estrogen) play a role, the primary biological causes of bipolar disorder involve chemicals that pass signals between neurons.
The Dopamine Dysregulation Hypothesis
Dopamine is the brain’s “reward” chemical.
- During Mania: There is evidence of excessive dopamine activity. This creates the feeling of euphoria, grandiosity, and the “need” to pursue rewards, even if they are risky.
- During Depression: Dopamine levels or sensitivity may drop, leading to anhedonia (the inability to feel pleasure).
Serotonin and Norepinephrine
- Serotonin: Known for regulating mood, sleep, and appetite. Imbalances here are closely linked to the depressive phases of the disorder.
- Norepinephrine: This chemical governs the “fight or flight” response. Excess norepinephrine is often linked to the physical agitation and racing thoughts found in mania.
Brain Structure & Circuitry Changes in Bipolar Disorder
Beyond just the “chemical soup,” what in the brain causes bipolar disorder also relates to the physical shape and health of certain circuits.
The Amygdala
This almond-shaped structure is the brain’s emotional alarm. In many people with bipolar disorder, the amygdala is physically different in size or density, making it “loud” and easily triggered.
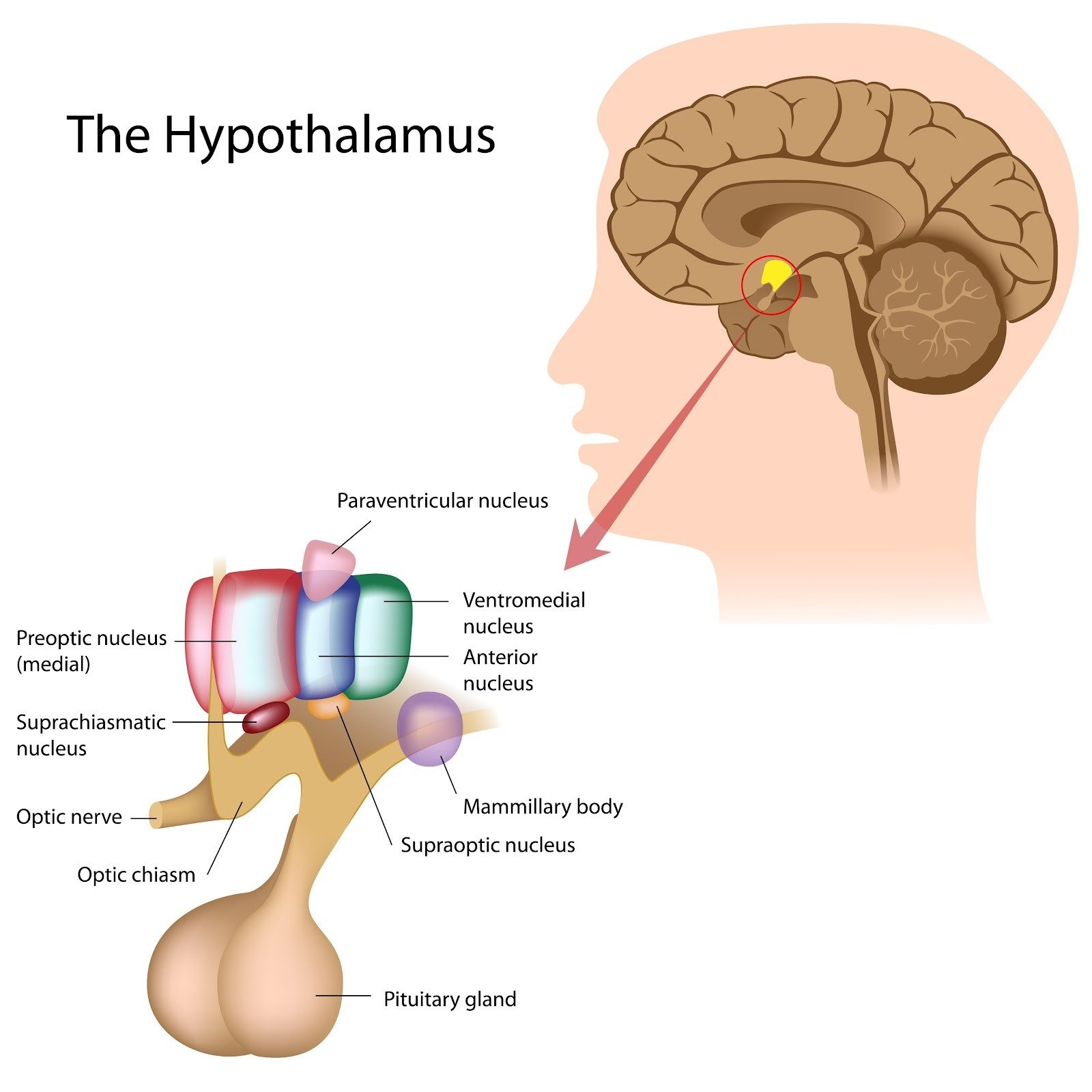
Circadian Rhythm Centers
The suprachiasmatic nucleus is the brain’s internal clock. Bipolar disorder is increasingly viewed by researchers as a “rhythm disorder.” The brain struggles to regulate the cycles of sleep, wakefulness, and body temperature. This is why sleep deprivation is one of the most powerful triggers for a manic episode—it breaks an already fragile internal clock.
Shutterstock
Explore
Genetics: Why Bipolar Runs in Families
Genetics is the most significant possible cause for bipolar disorder. Research involving twins shows that if one identical twin has bipolar disorder, there is a 40% to 70% chance the other will too.
Heritability Estimates
Bipolar disorder is one of the most heritable mental health conditions. However, it is not caused by a single “bipolar gene.” Instead, it involves hundreds of small genetic variations that, when added together, create a vulnerability.
Gene-Environment Interaction
Having the genes does not guarantee you will develop the disorder. Think of genes like “loading the gun,” while environment and stress “pull the trigger.” Many people carry the genetic markers for bipolar disorder but never experience an episode because their environment remains stable.
How Does Someone Become Bipolar? (Development Pathway)
One of the most frequent questions from parents and young adults is: how does someone become bipolar? The transition from a “healthy” brain to a clinical diagnosis is rarely an overnight event. It is usually a progressive journey involving a “perfect storm” of biological vulnerability and life circumstances.
Early Vulnerability Signs
Before a first full-blown episode, many people exhibit “prodromal” or early warning signs. These might include:
- Hypersensitivity: An unusually strong emotional reaction to small setbacks.
- Sleep Irregularity: Being a “night owl” who experiences extreme energy shifts based on sleep patterns.
- Cyclothymic Tendencies: Periods of being very “up” and productive followed by “slumps” that don’t yet meet the criteria for clinical depression.
The Stress-Activation Model
Scientists use the Diathesis-Stress Model to explain the onset. The “diathesis” is your genetic and biological predisposition (the “seeds”). The “stress” is the environmental factor (the “soil” and “weather”). You can have the seeds for bipolar disorder, but if the soil is never disturbed by high stress, trauma, or substance use, those seeds may never sprout.
First Episode Triggers
The first episode—often occurring in late teens or early twenties—is frequently triggered by a major life transition. The brain is undergoing significant pruning and development during this time. Common triggers include:
- Moving away to college.
- Severe grief or loss.
- Use of stimulants or hallucinogenic drugs.
- Intense sleep deprivation (often during finals or high-pressure work).
What Causes Bipolar Disorder to Get Worse Over Time?
A concerning question for many is what causes bipolar disorder to get worse. Unlike some conditions that stay stagnant, untreated bipolar disorder can be “progressive” due to a phenomenon known as the Kindling Effect.
The Kindling Effect
This theory suggests that the first few mood episodes are usually sparked by a major stressor (like a breakup). However, each episode “sensitizes” the brain. Over time, the threshold for an episode drops. Eventually, the brain can fire off a manic or depressive episode spontaneously, without any external trigger at all. This is why early intervention is so critical; it prevents the “kindling” from turning into a permanent fire.
Other Factors for Progression
- Substance Use: Alcohol and drugs act as “chemical stressors” that destabilize brain rhythms.
- Medication Non-compliance: Stopping and starting medications can sometimes lead to “refractory” bipolar disorder, where the brain becomes less responsive to treatments that previously worked.
- Chronic Sleep Disruption: Constant shift work or irregular sleep patterns can permanently damage the circadian rhythm centers.
Bipolar I vs. Bipolar II: Are Brain Causes Different?
While they share a name, the biological “flavor” of these two types differs.
- What is a Type 1 bipolar disorder? Bipolar I is defined by the severity of the “highs.” In the brain, this represents a massive surge in dopamine and a significant loss of “top-down” control from the prefrontal cortex, often leading to psychosis.
- What causes bipolar 2 disorder? Bipolar II is dominated by the “lows.” While hypomania is present, the biological “center of gravity” for Bipolar II is often in the depressive circuits. Research suggests Bipolar II may involve a more chronic, low-level inflammation in the brain compared to the acute “bursts” seen in Bipolar I.
How Bipolar Disorder Works Over Time (Mood Cycling Explained)
To understand how bipolar disorder works, imagine the brain’s mood regulation as a swinging pendulum. In a healthy brain, the pendulum swings in a narrow, controlled arc.
In the bipolar brain, the “hinge” of the pendulum is loose.
- Momentum: Once a manic episode gains momentum, it is very hard for the brain to stop it without chemical intervention.
- The Crash: After the high energy of mania is exhausted, the pendulum doesn’t stop at the center; the momentum carries it deep into the opposite side—depression. This is why mania is almost always followed by a “crash.”
How a Person With Bipolar Thinks (Brain-State Dependent Thinking)
One of the most fascinating (and frustrating) aspects of the disorder is how a person with bipolar disorder thinks. Because the brain’s “logic center” is physically impacted by mood states, their thoughts are often “state-dependent.”
- Manic Thinking: Thoughts are “fast” (racing thoughts). The brain makes connections that aren’t there (delusions of grandeur). The “risk-assessment” part of the brain is offline, so every idea feels like a “genius” idea.
- Depressive Thinking: Thoughts are “slow” and “heavy.” The brain filters out all positive memories, leaving only a “black-and-white” view of the world. The person may feel they have always been depressed, even if they were manic a week prior.
- Stable-State Thinking: When the brain chemistry is balanced, the person can look back at their manic or depressive thoughts with confusion, often saying, “I don’t know why I thought that.”
Is Bipolar Disorder Curable?
The most honest answer to whether bipolar disorder is curable is: No, but it is highly treatable.
Because the condition is rooted in the physical architecture and genetic coding of the brain, you cannot “wash it away” permanently. However, the brain is neuroplastic. This means you can “train” the brain to be more stable.
- Clinical Remission: With the right treatment, a person can go years, or even decades, without a significant episode. In the medical world, this is considered “success” rather than a “cure.”
Can Someone With Bipolar Be “Normal”? (Reassurance Section)
A common fear following a diagnosis is whether the individual will ever feel like themselves again. When people ask, “Can someone with bipolar disorder be normal?” they are usually asking if they can still hold a job, maintain a marriage, and experience genuine happiness.
The answer is a resounding yes. While your brain “processes” the world differently, “normalcy” is a spectrum. Many of the world’s most successful CEOs, artists, and parents live with bipolar disorder. Stability does not mean a life without emotion; it means having a brain that is resilient enough to handle those emotions without spiraling into a clinical crisis. With a combination of medical management and lifestyle discipline, the “bipolar brain” can function with incredible efficiency and creativity.
Triggers That Activate Bipolar Disorder in the Brain
While we have established what causes bipolar disorder in the brain biologically, we must also look at the external “keys” that unlock those biological states. Even with medication, certain possible causes for bipolar disorder to flare up remain.
- Sleep Deprivation: This is the #1 trigger. Missing even one night of sleep can “shock” the circadian rhythm, potentially launching a manic episode.
- High-Intensity Stress: Major life changes (even positive ones like a wedding or promotion) increase cortisol, which can disrupt neurotransmitter balance.
- Substance Use: Alcohol is a depressant, and stimulants (including excessive caffeine) mimic the “high” of mania, confusing the brain’s reward centers.
- Hormonal Shifts: For women, fluctuations in estrogen and progesterone during menstruation, pregnancy, or menopause can significantly impact mood stability.
Treatment of Bipolar Disorder: How Treatment Stabilizes the Brain
The treatment of bipolar disorder is designed to act as an external “support system” for the brain’s internal regulation.
Mood Stabilizers and Neural Regulation
Medications like Lithium or Valproate aren’t just “numbing” agents; they are neuroprotective.
- Lithium: It has been shown to physically increase gray matter in the brain and protect neurons from damage caused by the “stress” of mood episodes.
- Antipsychotics: These medications help “re-tune” dopamine receptors, preventing the sensory overload that leads to mania.
Therapy and Brain Pathways
Psychotherapy (like CBT or IPSRT) helps build “logical bypasses” in the brain. By learning to recognize the early signs of a mood shift, you are essentially training your prefrontal cortex to step in and manage the limbic system before the episode takes full control.
Frequently Asked Questions
Understanding the biological mechanics of the brain can be complex. Here are the most common questions regarding the neurological causes and effects of bipolar disorder.
What is the root cause of bipolar disorder?
There is no single root cause. Instead, it is the result of a “perfect storm” involving genetic predisposition (inheritance), neurochemical imbalances (neurotransmitters like dopamine), and environmental stressors that activate these biological vulnerabilities.
Is bipolar genetic or chemical?
It is a combination of both. Genetics provides the “blueprints” for how your brain is built, and those blueprints may include a sensitivity to certain chemical shifts. The “chemical” aspect refers to how those blueprints actually function day-to-day in your neurotransmitter systems.
Does bipolar disorder damage the brain?
Untreated, repeated, and severe mood episodes can lead to something called “cognitive scarring.” Research suggests that frequent manic or depressive episodes can cause wear and tear on the brain’s white matter and reduce gray matter density. However, consistent treatment—especially with mood stabilizers like Lithium—is considered neuroprotective, meaning it can help prevent and even repair this damage.
Can bipolar disorder improve with treatment?
Yes. While the underlying biological “wiring” remains, treatment helps the brain compensate. Medication balances the chemistry, while therapy strengthens the neural pathways between the logical prefrontal cortex and the emotional limbic system.
Is it a hormone imbalance?
While hormones (like cortisol from stress or estrogen during a menstrual cycle) can trigger episodes, bipolar disorder is primarily a disorder of neurotransmitters (the brain’s signaling chemicals) and circadian rhythms (the internal clock).
Why does sleep matter so much for the bipolar brain?
Bipolar disorder is often classified as a circadian rhythm disorder. The part of the brain that regulates sleep and energy—the suprachiasmatic nucleus—is hypersensitive. Sleep deprivation acts like a physical “shock” to this system, which can immediately flip the brain’s chemistry into mania.
Can someone be born with bipolar disorder?
A person can be born with the genetic vulnerability for bipolar disorder, but the symptoms typically do not appear until the brain undergoes significant developmental changes during late adolescence or early adulthood.
Conclusion
If there is one thing to carry away from this deep dive into the bipolar brain, it is this: bipolar disorder is a physical, biological reality. It is a condition of the organ known as the brain, just as diabetes is a condition of the pancreas.
Understanding that what causes bipolar disorder in the brain is a mix of faulty “wiring,” chemical surges, and genetic blueprints is the ultimate tool for destigmatization. When we view the disorder through a scientific lens, we move away from “What is wrong with you?” and toward “How can we stabilize your system?”
Bipolar disorder is challenging, but it is not a definition of your character. With the right medical support, lifestyle adjustments, and a commitment to brain health, you can lead a stable, vibrant, and profoundly “normal” life. The science of the brain is on your side, and recovery is a biological possibility.
Authoritative References
- National Institute of Mental Health (NIMH): The Neuroscience of Bipolar Disorder
- Brain & Behavior Research Foundation: Genetic Links in Bipolarity
- Mayo Clinic: Bipolar Brain Structure and Treatment Pathways
- Journal of Clinical Psychiatry: The Role of Neuroplasticity in Bipolar Recovery
- International Society for Bipolar Disorders (ISBD): Global Standards for Bipolar Management
Subscribe to Our Newsletter
Get mental health tips, updates, and resources delivered to your inbox.