Substance-Induced Mood Disorder: Symptoms, Diagnosis, and Treatment

The intersection of pharmacology and psychiatry is a complex landscape where the line between a primary mental health condition and the physiological effects of a substance often blurs. When an individual experiences profound emotional shifts—ranging from the depths of despair to the heights of euphoria—following the use of drugs, alcohol, or specific medications, they may be experiencing a substance-induced mood disorder (SIMD).
Understanding Substance-Induced Mood Disorder
To understand what a substance-induced mood disorder is, one must first recognize that the human brain is a delicate chemical ecosystem. Substances introduced into this system can mimic, block, or deplete neurotransmitters, leading to significant mood disturbances that are indistinguishable from naturally occurring depression or mania.
Recognizing the distinction between a substance-induced state and a primary mood disorder (such as Bipolar Disorder or Major Depressive Disorder) is critical for clinical success. Misdiagnosis can lead to inappropriate treatment, such as prescribing lifelong mood stabilizers for a condition that might resolve with abstinence, or conversely, failing to treat a lingering addiction that fuels psychiatric symptoms.
Commonly involved substances include alcohol, stimulants (like cocaine or methamphetamines), opioids, and even legitimate prescription medications like corticosteroids or interferon. This article provides a comprehensive exploration of SIMD, grounded in the latest 2026 clinical guidelines, to assist medical students, clinicians, and caregivers in navigating this intricate diagnosis.
Substance-Induced Mood Disorder
In the realm of clinical psychiatry, a substance-induced mood disorder definition describes a prominent and persistent disturbance in mood that is judged to be due to the direct physiological effects of a substance. This substance may be a drug of abuse, a medication, or a toxin.
According to the DSM-5-TR, the disorder manifests in two primary ways:
- Substance-Induced Depressive Disorder: Characterized by a pervasive low mood, loss of interest (anhedonia), and suicidal ideation occurring during or shortly after substance intoxication or withdrawal.
- Substance-Induced Bipolar and Related Disorder: Manifests as substance-induced mania or hypomania, featuring inflated self-esteem, racing thoughts, and decreased need for sleep.
Prevalence and Risk Factors
What is a substance-induced mental disorder in terms of population impact? It is remarkably common in emergency departments and addiction treatment centers. Research indicates that individuals with pre-existing biological vulnerabilities to mood disorders are at a higher risk. Furthermore, the “dual diagnosis” population—those already living with a primary mental illness—is significantly more susceptible to SIMD, as substances can act as a catalyst for latent psychiatric vulnerabilities.
Symptoms of Substance-Induced Mood Disorder
The substance-induced mood disorder symptoms are varied and depend heavily on the pharmacological profile of the substance involved. However, the hallmark is that these symptoms exceed what would normally be expected from simple intoxication or withdrawal.
Depressive Symptoms
When a substance triggers a depressive state, the clinical picture often mirrors Major Depressive Disorder.
- Persistent Sadness or “Empty” Mood: A deep sense of hopelessness.
- Anhedonia: A complete lack of interest in previously enjoyed activities.
- Fatigue and Lethargy: Significant physical and mental slowing (psychomotor retardation).
- Sleep Disturbances: Either insomnia or hypersomnia.
- Suicidal Ideation: Often acute and impulsive, particularly during withdrawal phases from stimulants or alcohol.
Manic and Hypomanic Symptoms
Substance-induced mania is most frequently associated with stimulants or specific medications.
- Euphoria or Irritability: An abnormally elevated or “edgy” mood.
- Decreased Need for Sleep: Feeling fully rested after only 2 or 3 hours of sleep.
- Grandiosity: Inflated self-esteem or “god-like” confidence.
- Risky Behavior: Excessive spending, hypersexuality, or dangerous driving.
- Pressured Speech: Talking faster than usual and being difficult to interrupt.
Acute vs. Chronic Effects
The timeline is essential. Acute symptoms may appear within minutes of intoxication (e.g., cocaine-induced euphoria), while chronic effects may develop over weeks of heavy use (e.g., alcohol-induced depression). It is the clinical persistence of these symptoms after the initial intoxication wears off that points toward a substance-induced mood disorder.
Causes and Risk Factors
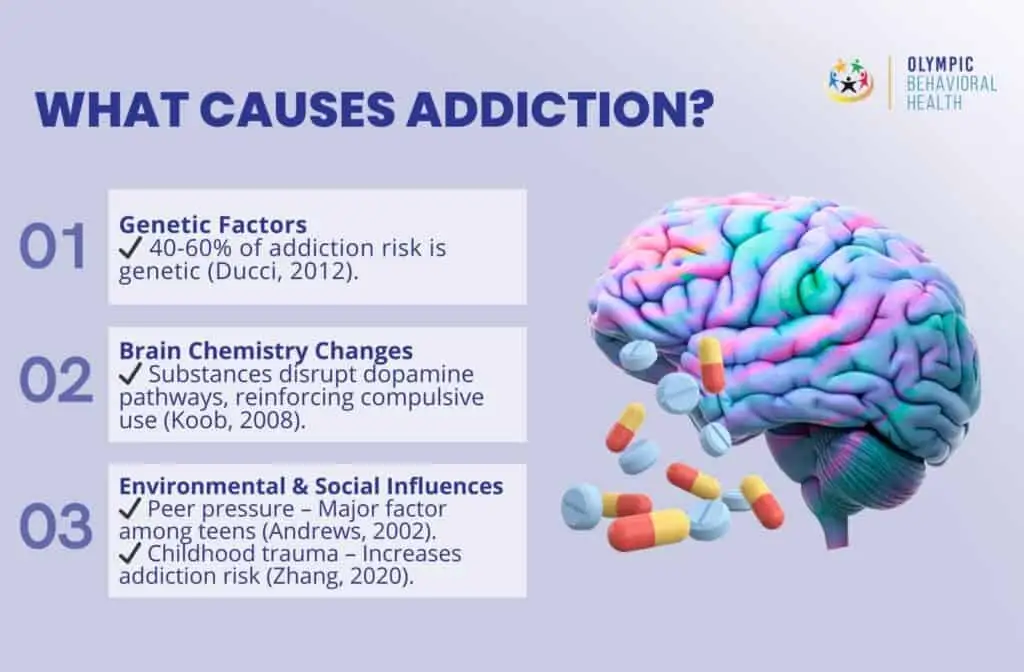
What causes substance-induced mental disorders? At the most basic level, it is the chemical alteration of the brain’s reward and regulatory centers. Substances alter the levels of dopamine, serotonin, and norepinephrine—the chemical messengers responsible for how we feel and react.
Commonly Implicated Substances
- Alcohol: Primarily a central nervous system depressant; long-term use frequently leads to chronic depressive states.
- Stimulants (Cocaine, Amphetamines): These drugs “flood” the brain with dopamine. During use, they cause mania; during the “crash,” they cause severe depression.
- Corticosteroids: Often used for physical ailments, these can induce “steroid psychosis” or mania.
- Opioids: While typically sedating, withdrawal often produces profound anxiety and depressive symptoms.
- What drugs make you act manic? Beyond illicit stimulants, medications like antidepressants (if used in a patient with latent bipolarity), phencyclidine (PCP), and even certain over-the-counter decongestants in high doses can trigger manic behavior.
Biological and Environmental Factors
Genetic predisposition plays a massive role. An example of a substance-induced disorder occurring in one person but not another can often be traced back to family history. If a person has a familial link to Bipolar Disorder, they are significantly more likely to experience stimulant-induced mania. Environmental triggers, such as high-stress environments or chronic pain, can also drive the patterns of use that lead to SIMD.
Diagnosis and Criteria
Navigating a substance-induced mood disorder diagnosis requires a meticulous “detective” approach by the clinician. The DSM-5 substance-induced mood disorder criteria provide a roadmap for this process.
DSM-5 Diagnostic Criteria
To meet the substance-induced mood disorder dsm 5 criteria, the following must be present:
- Mood Disturbance: A prominent and persistent disturbance in mood (depressed or elevated).
- Evidence of Cause: History, physical examination, or laboratory findings (toxicology) indicate that the symptoms developed during or soon after substance intoxication or withdrawal, or after exposure to a medication.
- Not Better Accounted For: The symptoms are not better explained by a primary mood disorder (e.g., the symptoms did not precede the onset of substance use).
- Clinical Distress: The disturbance causes significant distress or impairment in social, occupational, or other areas of functioning.
Differentiating Primary vs. Substance-Induced
The most challenging task is the “waiting game.” In many cases, a clinician must observe the patient during a period of abstinence (usually 4 weeks) to see if the symptoms remit.
- Timeline: If the symptoms persist longer than a month after acute withdrawal, the diagnosis may shift toward a primary mood disorder.
- History: A history of mood episodes during periods of prolonged sobriety strongly suggests a primary disorder.
- Mental Status Exam: Clinicians look for specific “markers”—for instance, the presence of certain types of hallucinations might point more toward a primary psychotic disorder or specific drug toxicities like PCP.
ICD-10 Classification and Codes
In the global medical community, the substance-induced mood disorder ICD-10 classification system serves as the universal language for clinical statistics, insurance billing, and health resource allocation. While the DSM-5-TR is primarily used for diagnostic clinical interviews, the ICD-10 (International Classification of Diseases, 10th Revision) is the backbone of the administrative and epidemiological world.
Unlike the DSM-5, which often groups these disturbances under a singular conceptual umbrella, the ICD-10 utilizes a granular, multi-axial “F-code” system. This granularity is essential because the physiological trajectory of an alcohol-induced depressive state is vastly different from that of a methamphetamine-induced manic episode.
The Hierarchical Structure of the F-Code
The ICD-10 code for substance-induced mood disorder is found within the block of codes F10–F19, which covers “Mental and behavioral disorders due to psychoactive substance use.” The structure follows a logical F1x.xx format:
- The Second and Third Digits (F1x): These identify the specific substance responsible for the mood disturbance.
- The Fourth Digit (.9): In many coding instances, the digit after the decimal indicates the severity or specific clinical manifestation—in this case, “unspecified” or “induced” use.
- The Fifth Digit (.x4): Specifically denotes the presence of a mood disorder.
Detailed ICD-10 Code Breakdown
To ensure clinical accuracy and proper substance-induced mood disorder (HCC) ICD-10 reporting, clinicians must use the code that corresponds to the primary substance involved:
- F10.94: Alcohol-induced mood disorder (often presenting as profound depression).
- F11.94: Opioid-induced mood disorder (often manifesting during acute withdrawal).
- F12.94: Cannabis-induced mood disorder (can present as anxiety or depressive symptoms).
- F13.94: Sedative, hypnotic, or anxiolytic-induced mood disorder.
- F14.94: Cocaine-induced mood disorder (frequently associated with substance-induced mania).
- F15.94: Other stimulant-induced mood disorder (includes amphetamines, methamphetamines, and even high-dose caffeine).
- F16.94: Hallucinogen-induced mood disorder.
- F19.94: Other psychoactive substance-induced mood disorder (vital for “polysubstance” users where the exact primary driver is unclear).
HCC Coding and Clinical Relevance
For healthcare administrators and insurers, the ICD-10 substance-induced mood disorder designation is linked to Hierarchical Condition Categories (HCC). These categories are critical for “risk adjustment”—a process that predicts the cost of care for a patient.
Because SIMD often requires a “dual diagnosis” approach—meaning the patient needs both addiction counseling and psychiatric intervention—it carries a higher “acuity” score. Accurate coding ensures that a hospital or clinic receives the proper funding to provide integrated care, which often includes a multidisciplinary team of detox specialists, psychiatrists, and social workers. Furthermore, precise coding in the EHR (Electronic Health Record) allows for better longitudinal tracking; for instance, if a patient has multiple F14.94 (Cocaine-induced mania) admissions, it alerts the clinical team to a severe, recurring pattern that may require more intensive residential treatment rather than standard outpatient care.
Substance-Induced Mood Disorder vs. Primary Mood Disorders
Distinguishing between substance-induced mood disorder and bipolar or major depression is one of the most difficult tasks in emergency psychiatry. The difference between substance-induced and primary mood disorder primarily hinges on the “temporal relationship”—the timing of when symptoms appear and disappear relative to drug use.
Key Differentiating Factors
- Symptom Onset: In SIMD, symptoms typically develop during or within 30 days of substance use or withdrawal. In a primary disorder, symptoms often exist independently of substance use history.
- The “Washout” Period: This is the gold standard for diagnosis. If mood symptoms evaporate after a period of supervised sobriety (usually 2 to 4 weeks), the diagnosis is confirmed as substance-induced.
- Age of Onset: Primary bipolar disorder often emerges in late adolescence or early 20s. If a 45-year-old with no prior psychiatric history suddenly presents with mania after starting a new medication or using cocaine, SIMD is the statistically more likely culprit.
The Risk of Misdiagnosis
Mislabeling a patient can have long-term consequences. A patient with substance-induced depression who is misdiagnosed with Major Depressive Disorder might be prescribed antidepressants that could potentially trigger a manic switch if the “depression” was actually part of a stimulant-withdrawal cycle. Conversely, labeling a primary bipolar patient as “just a drug user” can deny them the life-saving mood stabilizers they need to stay stable and sober.
Treatment Approaches
Effective substance-induced mood disorder treatment must be dual-faceted. It is not enough to treat the mood; one must also address the chemical driver of that mood. How to treat substance-induced mood disorder effectively requires a combination of immediate stabilization and long-term behavioral change.
Acute Management and Detoxification
The first priority is safety and stabilization.
- Detoxification: If the mood disorder is driven by alcohol, opioids, or benzodiazepines, a medically supervised detox is necessary to manage life-threatening withdrawal symptoms that exacerbate mood swings.
- Safety Assessment: Given the high impulsivity associated with substance-induced mania and the deep hopelessness of induced depression, inpatient hospitalization may be required to prevent self-harm or risky behaviors.
Pharmacological Treatment
Medication use in SIMD is often temporary and highly specific:
- Antipsychotics: Low-dose atypical antipsychotics may be used acutely to “dampen” substance-induced mania or agitation.
- Mood Stabilizers: These are generally reserved for cases where symptoms do not resolve after detoxification, suggesting an underlying primary bipolar disorder triggered by the substance.
- Antidepressant Cautions: Clinicians are often hesitant to use SSRIs during the acute withdrawal phase of stimulant abuse, as the brain’s receptors are already in a state of flux.
Psychotherapy and Integrated Care
The most successful outcomes result from integrated care, where psychiatric and addiction treatments happen simultaneously.
- Cognitive Behavioral Therapy (CBT): Helps patients identify the thoughts that lead to substance use and the subsequent mood crashes.
- Motivational Interviewing (MI): An evidence-based approach to help patients find internal motivation to cease the substance use driving their mood disorder.
- Relapse Prevention: Teaching the patient that a “slip” in sobriety will likely lead to a recurrence of the painful mood symptoms.
Prognosis and Recovery

A common question from families is: “Does substance-induced mood disorder go away?” The answer is generally optimistic, but it depends on the “reversibility” of the damage.
Short-Term vs. Long-Term Outcomes
For many, the prognosis is excellent. Once the offending substance is removed and the brain’s neurochemistry returns to equilibrium (homeostasis), the mood disorder often resolves completely.
However, substance-induced mood disorder long-term outcomes can be complicated by:
- Neurotoxicity: Heavy, long-term use of stimulants (like methamphetamines) can cause semi-permanent changes to dopamine transporters, leading to lingering depressive symptoms or “anhedonia” that lasts for months or even years.
- Kindling Effect: Repeated cycles of substance-induced mania can make the brain more sensitive, eventually leading to the development of a permanent, primary bipolar disorder.
Recovery is not just about the absence of symptoms; it is about the restoration of function. Adherence to a recovery program and ongoing mental health monitoring are the best predictors of a “one-time” episode versus a chronic psychiatric struggle.
Common Examples and Case Studies
To contextualize the clinical data, observing an example of a substance-induced disorder in practice helps illustrate the high stakes of accurate diagnosis. These scenarios represent the most frequent presentations in modern clinical settings.
Alcohol-Induced Depressive Disorder
A 45-year-old male presents with symptoms that mirror Major Depressive Disorder: profound lethargy, morning tearfulness, and passive suicidal ideation. He has been drinking heavily (10–12 units daily) for six months.
- The Diagnostic Clue: The patient reports that his mood was stable prior to the increase in alcohol consumption.
- Outcome: Following a supervised detox and three weeks of abstinence, his “depression” scores dropped significantly without the use of antidepressants, confirming a substance-induced etiology.
Stimulant-Induced Mania
A college student is brought to the ER exhibiting classic signs of substance-induced mania: rapid-fire speech, spending his entire tuition on cryptocurrency, and going 72 hours without sleep. A toxicology screen is positive for amphetamines (prescribed for ADHD but misused).
- The Diagnostic Clue: The symptoms are far more intense than typical ADHD and emerged only after he began doubling his dose for final exams.
- Outcome: Once the stimulant is cleared from his system and he receives two nights of medically assisted sleep, the “manic” behavior resolves.
Prescription Medication-Induced Changes
Not all SIMD cases involve illicit “drugs that trigger mood episodes.” A patient being treated with high-dose Prednisone for an autoimmune flare-up may suddenly experience severe irritability and grandiosity. In this case, the “substance” is a necessary medical treatment, requiring the clinician to balance psychiatric stabilization with the patient’s physical health needs.
Frequently Asked Questions
What is a substance-induced mood disorder?
It is a clinical condition where an individual experiences significant symptoms of depression or mania caused directly by the physiological effects of a drug, alcohol, or medication. Unlike a primary mood disorder, the symptoms are fundamentally tied to the presence or withdrawal of the chemical.
What are the symptoms of a substance-induced mood disorder?
Symptoms vary based on the drug. Substance-induced depressive disorder includes low mood, fatigue, and loss of interest. Substance-induced mania involves euphoria, racing thoughts, decreased need for sleep, and impulsive, risky behaviors.
What causes substance-induced mental disorders?
The primary cause is the alteration of neurotransmitters in the brain, such as dopamine and serotonin. Substances can “hijack” these pathways, leading to emotional extremes that the brain cannot regulate on its own.
Does substance-induced mood disorder go away?
In most cases, yes. If the brain has not suffered significant neurotoxic damage, the mood disorder typically remits once the substance is completely cleared from the body and a period of sobriety is maintained.
What drugs make you act manic?
The most common culprits are stimulants (cocaine, methamphetamines, MDMA), certain antidepressants (in susceptible individuals), corticosteroids (steroids), and high-dose ADHD medications.
How is the ICD-10 code used for this diagnosis?
The substance-induced mood disorder icd 10 code (such as F10.94 for alcohol) is used by clinicians to specify the cause of the mood shift. This ensures the patient receives the correct integrated treatment for both the psychiatric symptoms and the underlying substance use.
Conclusion
A substance-induced mood disorder is a high-stakes psychiatric condition that requires a sophisticated, non-judgmental approach to diagnosis and treatment. As we have explored, the hallmark of SIMD is its direct relationship to chemical exposure, whether through illicit drug use, alcohol, or prescription medication.
The journey to recovery hinges on early recognition. By utilizing the substance induced mood disorder dsm 5 criteria and appropriate icd 10 substance induced mood disorder coding, clinicians can ensure that patients are not just treated for their mood, but are given the tools to address the substance use at the heart of the problem.
With substance-induced mood disorder treatment that integrates detoxification, evidence-based psychotherapy like CBT, and long-term relapse prevention, the vast majority of individuals can return to a state of emotional equilibrium. The brain possesses a remarkable capacity for healing; once the chemical interference is removed, the path back to a stable, healthy life becomes clear.
Authoritative References
1. StatPearls (NCBI/NIH) – Substance-Induced Depressive Disorder
2. ICD-10 Data – Mental and Behavioral Disorders (F10-F19)
3. SAMHSA – Treatment for Co-Occurring Disorders
4. American Psychiatric Association (APA) – Understanding Bipolar and Related Disorders
5. Mayo Clinic – Drug-Induced Mania and Depression
Subscribe to Our Newsletter
Get mental health tips, updates, and resources delivered to your inbox.










