Dialectical Behavior Therapy (DBT) for Borderline Personality Disorder
For decades, Borderline Personality Disorder (BPD) was shrouded in clinical pessimism. It was frequently labeled as “untreatable,” and patients were often marginalized by a healthcare system that lacked the specific tools to address the profound emotional dysregulation and high-risk behaviors associated with the diagnosis. This changed with the emergence of dialectical behavior therapy for borderline personality disorder.
Today, DBT is recognized globally as the gold standard of care. It has transformed BPD from a “hopeless” label into a manageable condition with high rates of remission. Unlike traditional talk therapies that may inadvertently invalidate a patient’s intense pain, DBT provides a structured, compassionate, and evidence-based roadmap. It doesn’t just aim to suppress symptoms; it aims to help individuals build a “life worth living.”
What Is Dialectical Behavior Therapy?
At its core, dialectical therapy for borderline personality disorder is a specialized form of cognitive-behavioral therapy (CBT) that emphasizes the social and emotional aspects of living. The term “dialectical” refers to the philosophical concept of balancing two seemingly opposite ideas: Acceptance and Change.
In DBT, the therapist and patient work together to accept the patient’s feelings and experiences as valid in the moment, while simultaneously acknowledging that the patient must change their behaviors to move forward.
The Six Foundational Principles of DBT
Understanding what the six main points of dialectical behavior therapy (often referred to as its foundational assumptions) are is key to understanding its method:
- The Biosocial Theory: BPD is viewed as a biological predisposition to emotional sensitivity exacerbated by an invalidating environment.
- Dialectics: The universe is filled with opposing forces that must be balanced.
- Core Mindfulness: The practice of being fully present without judgment.
- Behavioral Analysis: Every action has a cause; by analyzing the “chain” of events, we can find points for intervention.
- Validation: Accepting the patient’s internal reality as understandable, given their history.
- Continuous Assessment: Therapy is constantly monitored and adjusted based on real-world data and progress.
Who Founded Dialectical Behavior Therapy?
The dialectical behavior therapy founder is Dr. Marsha M. Linehan, a clinical psychologist whose personal history is as influential as her academic prowess. In the 1970s and 80s, Linehan realized that standard CBT was often too focused on change, which felt invalidating to BPD patients, leading them to drop out of treatment.
Dr. Linehan’s breakthrough came when she incorporated Zen mindfulness and radical acceptance into behavioral science. In a landmark 2011 disclosure, Linehan revealed her own history of severe BPD-related struggles, including self-harm and hospitalization.
Her lived experience ensured that DBT was designed not from an ivory tower, but from a place of deep, empathetic understanding of what it feels like to live with a “thin skin” in a world of triggers.
DSM-5 Criteria for Borderline Personality Disorder
To appreciate why DBT with borderline personality disorder is so effective, one must understand the symptoms it targets. The Diagnostic and Statistical Manual of Mental Disorders (DSM-5) defines BPD through nine specific criteria. A diagnosis typically requires meeting at least five of the following:
- Frantic efforts to avoid real or imagined abandonment.
- A pattern of unstable and intense interpersonal relationships (often characterized by “splitting”).
- Identity disturbance: Markedly unstable self-image or sense of self.
- Impulsivity in at least two areas that are potentially self-damaging (e.g., spending, substance abuse, reckless driving).
- Recurrent suicidal behavior, gestures, or threats, or self-mutilating behavior.
- Affective instability: Intense, rapid mood swings.
- Chronic feelings of emptiness.
- Inappropriate, intense anger or difficulty controlling anger.
- Transient, stress-related paranoid ideation or severe dissociative symptoms.
DBT is uniquely structured to “match” these symptoms with specific behavioral skills, ensuring that every diagnostic challenge has a clinical solution.
Why DBT Was Designed Specifically for Borderline Personality Disorder
While DBT is now used for eating disorders, PTSD, and substance abuse, it was originally developed as a targeted dbt treatment for BPD. The reason for this specialization lies in the “Biosocial Model.”
Linehan posited that individuals with BPD are born with an “emotional thermostat” that is set significantly higher than that of others. They feel emotions faster, more intensely, and take longer to return to a baseline state. When this biological vulnerability meets an “invalidating environment”—one where a child’s emotions are punished, ignored, or mocked—the result is a catastrophic failure in emotional regulation.
Addressing Therapy-Interfering Behaviors
One of the primary reasons BPD was considered “difficult to treat” was the frequency of self-harm and therapy drop-outs. DBT addresses this by prioritizing “therapy-interfering behaviors.” If a patient is missing sessions or acting out, the therapist addresses those behaviors first, ensuring the therapeutic container remains stable enough for long-term work.
DBT Therapy Structure: How DBT Actually Works
For a program to be considered “comprehensive DBT,” it must include four specific components. Each part of dialectical behavior therapy (dbt) matches a specific application to ensure the patient is supported 24/7.
| DBT Component | Application / Function |
| Individual Therapy | Focused on motivation, safety, and applying skills to the specific events of the past week. |
| Skills Training Group | A classroom-like setting where patients learn the “how-to” of mindfulness, distress tolerance, and more. |
| Phone Coaching | Real-time support where patients call their therapist before acting on a crisis urge to get help applying a skill. |
| Consultation Team | A “therapy for the therapists” meeting to prevent burnout and ensure the clinical team remains dialectical. |
This multi-modal approach ensures that the patient isn’t just “talking about their feelings” once a week, but is actively re-training their brain and behavior in every area of their life.
DBT Skills for Borderline Personality Disorder
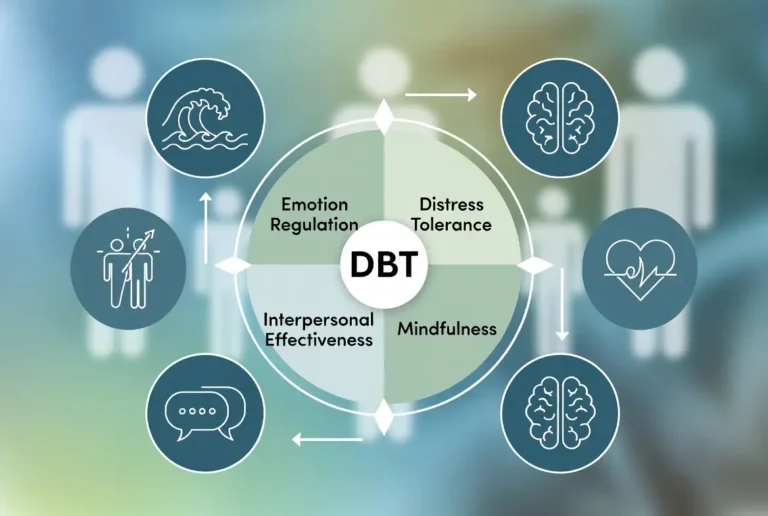
The “heart” of DBT skills for borderline personality is divided into four modules. These represent the 4 techniques of DBT that every patient must master to achieve remission.
1. Mindfulness
The foundation of all other skills. It teaches patients to observe their thoughts and feelings without judgment. Instead of being in the emotion, they learn to view the emotion.
- Example: Using “Wise Mind”—the balance between the “Rational Mind” and the “Emotional Mind.”
2. Distress Tolerance
Specifically for crisis situations. These are “survival” skills to get through an emotional storm without making the situation worse (e.g., avoiding self-harm).
- Example: The TIPP skill (Temperature, Intense Exercise, Paced Breathing, Paired Muscle Relaxation) to physically lower the body’s arousal level.
3. Emotion Regulation
These skills help reduce the overall vulnerability to “emotional hijacking.” Patients learn to label emotions and “check the facts” to see if their emotional intensity matches the situation.
- Example: “Opposite Action”—if you feel the urge to isolate (fear), you purposefully move toward people.
4. Interpersonal Effectiveness
Focuses on maintaining relationships while respecting oneself. It provides scripts for how to ask for what you need or say “no” without blowing up a relationship.
- Example: DEAR MAN (Describe, Express, Assert, Reinforce, Mindful, Appear Confident, Negotiate).
What Are the 3 C’s of BPD — and How DBT Addresses Them?

The 3 C’s Explained in Detail
- I didn’t cause it. BPD arises from a complex interplay of factors: genetic predisposition (e.g., heightened emotional sensitivity), neurobiological differences in emotion regulation areas of the brain, and environmental influences like childhood invalidation, trauma, abuse, neglect, or unstable attachments. No single person — parent, partner, friend, or caregiver — “causes” the disorder through their actions or inactions. Loved ones often internalize intense blame (“If only I had been more patient/affectionate/stable…”), especially when behaviors involve anger, accusations, or self-harm. This self-blame fuels cycles of over-responsibility and resentment. Recognizing “I didn’t cause it” releases unnecessary guilt, allowing supporters to respond from clarity rather than defensiveness or shame.
- I can’t control it. Emotional dysregulation, fear of abandonment, black-and-white thinking (“splitting”), impulsivity, and intense mood shifts are core BPD symptoms. These are internal experiences rooted in the person’s biology and history — no amount of pleading, fixing, enabling, or “walking on eggshells” can force regulation or prevent episodes. Attempts to control often backfire, escalating conflict or reinforcing dependency. This C empowers boundaries: You can influence your own responses (e.g., validating feelings without endorsing harmful actions), but you cannot dictate someone else’s internal state or choices. It shifts focus from “How do I stop this?” to “How do I protect my well-being while offering support?”
- I can’t cure it. BPD is treatable — many achieve significant remission or “recovery” (defined as reduced symptoms, stable relationships, and fulfilling lives) — but healing requires the person’s active commitment to evidence-based treatment, self-awareness, and consistent practice. No external “rescue” (love, ultimatums, endless accommodation) substitutes for that internal work. This truth combats the exhausting “fixer” role common in relationships with BPD, where supporters pour energy into motivating therapy, managing crises, or shielding from consequences — often at great personal cost. Accepting “I can’t cure it” encourages realistic hope: Professional help (especially DBT) works best when the individual owns their recovery.
These principles, sometimes expanded to “3 C’s and 3 G’s” (Get off their back, Get out of the way, Get on with your own life), draw from Al-Anon and codependency recovery models but are frequently applied to BPD family dynamics. They promote self-care, reduce enabling, and foster healthier interactions.
How DBT Addresses the 3 C’s Through Radical Acceptance
Dialectical Behavior Therapy (DBT) — the gold-standard, evidence-based treatment for BPD, developed by Dr. Marsha Linehan (who herself recovered from severe BPD symptoms) — directly aligns with the 3 C’s via its core skill of Radical Acceptance. This acceptance-based strategy teaches both individuals with BPD and their loved ones to acknowledge painful realities without judgment, resistance, or futile attempts to change what cannot be changed.
- For the person with BPD: Radical Acceptance counters self-blame (“I caused my own pain”) and helplessness by accepting the biosocial origins of their disorder (biology + invalidating environment) while committing to change what is possible (behaviors, skills).
- DBT’s modules — Mindfulness (observing emotions without fusion), Distress Tolerance (surviving crises without escalation), Emotion Regulation (reducing vulnerability), and Interpersonal Effectiveness (assertive communication) — build the internal tools needed for self-directed recovery. This empowers the individual to take ownership, reducing reliance on others to “fix” them.
- For loved ones and families: DBT often includes family skills training or parallel support (e.g., Family Connections programs). Radical Acceptance helps supporters embrace the 3 C’s: Accept that BPD exists (no causation guilt), that symptoms are not fully controllable by external forces, and that cure/recovery is the person’s journey (not a personal failure if progress is slow). This frees energy for validation (“I see you’re in pain”), consistent boundaries, and self-care — creating a validating environment that actually supports treatment adherence rather than enabling avoidance.
In essence, the 3 C’s provide a liberating mantra for supporters, while DBT’s Radical Acceptance operationalizes them into actionable skills. Together, they shift the narrative from blame/fixation to compassionate realism: BPD is serious but manageable, recovery is possible with commitment, and everyone involved deserves well-being.
Is Dialectical Behavior Therapy Effective for BPD?
When patients or clinicians ask, “Is dialectical behavior therapy effective for borderline personality disorder (BPD)?” the answer is supported by decades of clinical trials. DBT was the first psychotherapy shown to be effective for BPD in controlled studies.
Evidence and Outcomes
The effectiveness of DBT for borderline personality disorder is measured by several key metrics:
- Reduction in Self-Harm: DBT consistently shows a significant decrease in “parasuicidal” behaviors and emergency room visits.
- Improved Retention: Because of the emphasis on validation, patients stay in DBT longer than in traditional CBT.
- Fewer Hospitalizations: Studies show that DBT graduates spend significantly less time in inpatient psychiatric units.
According to a 2024 meta-analysis, the effectiveness of dialectical behavior therapy is answered with a high “effect size,” meaning the improvements are robust and long-lasting, often leading to full diagnostic remission.
DBT vs CBT for Borderline Personality Disorder

A common question in academic and clinical circles is: “Can cognitive behavioral therapy improve symptoms of borderline personality disorder (BPD)?” While CBT is excellent for depression and anxiety, it often falls short for BPD.
Why DBT Expanded CBT
Standard CBT focuses heavily on identifying and correcting “distorted” thoughts. For a person with BPD, being told their thoughts are “wrong” or “distorted” can feel like a repeat of the invalidating environment that caused their trauma.
- Validation: DBT adds a layer of validation that CBT lacks.
- Dialectics: DBT focuses on the balance between acceptance and change, whereas CBT is almost exclusively focused on change.
- Support: DBT offers phone coaching and consultation teams, which are not standard in CBT frameworks.
Is DBT a Cure for Borderline Personality Disorder?
It is vital to be realistic: Is DBT a cure for borderline personality disorder? In the medical sense, no. Personality disorders are not “cured” like an infection; they are managed until they reach remission.
Remission vs. Cure
Remission means the patient no longer meets the DSM-5 criteria for the disorder. Their “emotional thermostat” might still be sensitive, but they have the skills to handle it without self-destruction. Recovery is a journey of moving from “hell” to a “life worth living.”
DBT Techniques in Action
To understand dialectical behavior therapy examples, we look at how skills are applied in the heat of the moment.
- Managing Splitting: A patient feels their therapist hates them because they were 5 minutes late. Instead of ghosting the therapy, the patient uses “Checking the Facts” to see if there is actual evidence of hatred.
- Crisis Survival: A person feels a massive urge to self-harm. Instead of acting, they use the TIPP skill, plunging their face into cold water to reset their nervous system.
- Conflict Repair: After an argument with a partner, the patient uses the GIVE skill (Gentle, Interested, Validate, Easy manner) to de-escalate the tension rather than lashing out.
Frequently Asked Questions
Is dialectical behavior therapy effective for BPD?
Yes. It is the most researched and validated treatment for BPD, specifically effective at reducing self-harm and hospitalization.
What are the 4 techniques of DBT?
The four core modules are Mindfulness, Distress Tolerance, Emotion Regulation, and Interpersonal Effectiveness.
What are the 7 crucial DBT strategies?
These typically refer to core clinical strategies: Validation, Problem Solving, Irreverent Communication, Consultant to the Patient, Dialectical Strategies, Commitment Strategies, and Chain Analysis.
Can CBT help borderline personality disorder?
CBT can help with specific symptoms like depression, but it lacks the validation and crisis support needed to treat the core features of BPD effectively.
Conclusion
DBT changed the trajectory of mental health history by proving that people with BPD can recover. It replaced blame with skills and replaced “management” with a “life worth living.” While the work is intensive and requires a high level of commitment, the results—a stable sense of self and healthy, lasting relationships—are worth every effort.
If you or a loved one is struggling, remember that BPD is a set of learned behaviors and biological sensitivities, both of which can be retrained. Recovery is not just a hope; in the world of DBT, it is a documented reality.
Authoritative References
1. Behavioral Tech (A Linehan Institute Training Company)
2. American Psychiatric Association (APA) –Practice Guidelines
3. National Institute of Mental Health (NIMH) – BPD Research
4. The Cochrane Library – Systematic Reviews of BPD Treatments
5. National Education Alliance for Borderline Personality Disorder (NEABPD)
Subscribe to Our Newsletter
Get mental health tips, updates, and resources delivered to your inbox.