What is the best therapy for Bipolar Disorder? Evidence-Based Treatments, Goals & Real-Life Management

Navigating a diagnosis of bipolar disorder can feel like being caught in an emotional tug-of-war. One moment, you may feel an unstoppable surge of energy; the next, you are anchored by the weight of a profound depression. When faced with these extremes, the most urgent question for patients and families is: What therapy is best for bipolar disorder?
As we move through 2026, the clinical landscape for mental health has become more personalized than ever. We now understand that there is no “one-size-fits-all” answer. The best therapy for bipolar disorder is a tailored strategy that accounts for your specific subtype—whether Bipolar I or Bipolar II—your unique triggers, and your lifestyle. While medication often provides the biological foundation, psychotherapy is the “architecture” that helps you build a stable, functional life.
In this comprehensive guide, we will explore the gold standard treatment for bipolar disorder, dive into the most effective therapy modalities like CBT and IPSRT, and provide actionable advice for long-term recovery. Whether you are looking for the recommended treatment for bipolar or wondering if a “normal” life is truly possible, this guide serves as your evidence-based roadmap.
What Is the Gold Standard Treatment for Bipolar Disorder?
In the world of psychiatry, “gold standard” refers to the treatment approach that has the highest level of scientific evidence for success. For bipolar disorder, that standard is unequivocally the combination treatment model.
The Synergy of Medication and Psychotherapy
Bipolar disorder is fundamentally a biological condition involving neurotransmitter dysregulation and circadian rhythm sensitivity. Because of this, clinical guidelines from major organizations—such as the American Psychiatric Association (APA) and the International Society for Bipolar Disorders (ISBD)—consistently name the pairing of pharmacotherapy (medication) and evidence-based psychotherapy as the most effective treatment for bipolar disorder.
- Medication acts as the “floor” and “ceiling.” It prevents you from falling too deep into depression and stops you from rising too high into mania.
- Psychotherapy provides the “walls.” it teaches you how to navigate the space in between, recognize early warning signs, and manage the wreckage that mood episodes can leave behind in your relationships and career.
Why Long-Term Management Is Essential
Bipolar disorder is a chronic, lifelong condition. Unlike a localized infection that you treat for ten days, bipolar disorder requires a maintenance mindset. The recommended treatment for bipolar disorder involves shifting from “crisis management” (treating an episode once it happens) to “prophylactic care” (preventing the next episode from ever starting).
Treatment Goals for Bipolar Disorder
Before deciding what kind of therapy is best for bipolar disorder, it is helpful to define what “success” looks like. In 2026, clinicians have moved beyond just “stopping the swings.” Modern treatment goals for bipolar disorder are focused on functional recovery.
Primary Objectives
- Mood Stabilization: Reducing the frequency, intensity, and duration of manic, hypomanic, and depressive episodes.
- Relapse Prevention: Developing a “relapse signature”—a personalized list of early warning signs (like sleeping two hours less or talking faster) to catch an episode before it escalates.
- Functional Recovery: Ensuring you can hold a job, maintain healthy relationships, and attend to daily responsibilities.
- Quality of Life and Autonomy: Empowering you to make choices about your life that are not dictated by your symptoms.
Bipolar 1 vs Bipolar 2: How Treatment & Therapy Differ
The type of bipolar disorder you have significantly influences what type of therapy is best for you. While the core principles remain the same, the “target” of the therapy often shifts.
Bipolar I: Managing Mania and Relapse Risk
Bipolar I is characterized by full manic episodes that may involve psychosis or require hospitalization.
- Therapy Focus: Because mania can be destructive to one’s life and safety, therapy often focuses heavily on relapse prevention and medication adherence.
- Key Challenge: Many people enjoy the early stages of mania (hypomania), making it difficult to want to “stop” the climb. Therapy helps build the insight necessary to recognize that the “high” always comes with a devastating “low.”
Bipolar II: Treating Depression and Mood Instability
Bipolar II involves hypomania (milder highs) and much more frequent, lingering depressive episodes.
- Best Treatment for Bipolar 2: Since depression is the dominant feature, bipolar 2 treatment options often lean toward therapies that target chronic low mood and the anxiety that frequently accompanies it.
- Key Challenge: Bipolar II is often misdiagnosed as standard clinical depression. Therapy for Bipolar II must include a heavy dose of psychoeducation so the patient can distinguish between their “best self” and a hypomanic state.
Best Therapy Modalities for Bipolar Disorder

This is the core of your treatment plan. Research has identified several best therapy modalities for bipolar disorder that consistently outperform general “talk therapy.”
4.1 Cognitive Behavioral Therapy (CBT)
Cognitive behavioral therapy for bipolar disorder is perhaps the most famous and widely available option. It works on the principle that your thoughts, feelings, and behaviors are all interconnected.
- Thought Restructuring: Learning to challenge “automatic” thoughts. During depression, you might think, “I’ll never be happy again.” CBT helps you see this as a symptom of the illness, not a permanent truth.
- Behavioral Activation: In depressive states, CBT encourages small, manageable actions to break the cycle of lethargy.
- Relapse Prevention: One of the most vital uses of CBT in bipolar care is creating a “mood map” to track energy levels and identify triggers.
4.2 Interpersonal and Social Rhythm Therapy (IPSRT)
If you ask a specialist what therapy is best for bipolar disorder, they will often point to IPSRT. This therapy is specifically designed for the bipolar brain’s sensitivity to routine.
- The “Social Rhythm” Factor: IPSRT focuses on stabilizing your “social zeitgebers”—daily events like when you wake up, eat lunch, and go to bed.
- The Circadian Connection: Since sleep disruption is the #1 trigger for mania, IPSRT teaches you to guard your sleep-wake cycle with absolute discipline.
- Interpersonal Stability: It also addresses the stress in your relationships, as conflict is a major trigger for mood shifts.
4.3 Family-Focused Therapy (FFT)
Bipolar disorder doesn’t just happen to an individual; it happens to a family. Family-focused therapy for bipolar disorder involves loved ones in the treatment process.
- Education for All: Family members learn the biological nature of the disorder, reducing the “why can’t you just get over it?” friction.
- Communication Training: Learning how to express concern without being overbearing or triggering “high expressed emotion” (criticism or hostility), which is a proven trigger for relapse.
- Crisis Planning: Working as a team to decide exactly what will happen if a manic or depressive episode begins.
4.4 Other Supportive Therapies
- Psychoeducation: Often delivered in groups, this is a structured way to learn the “mechanics” of your illness. Knowledge is the ultimate tool for reducing the shame associated with the diagnosis.
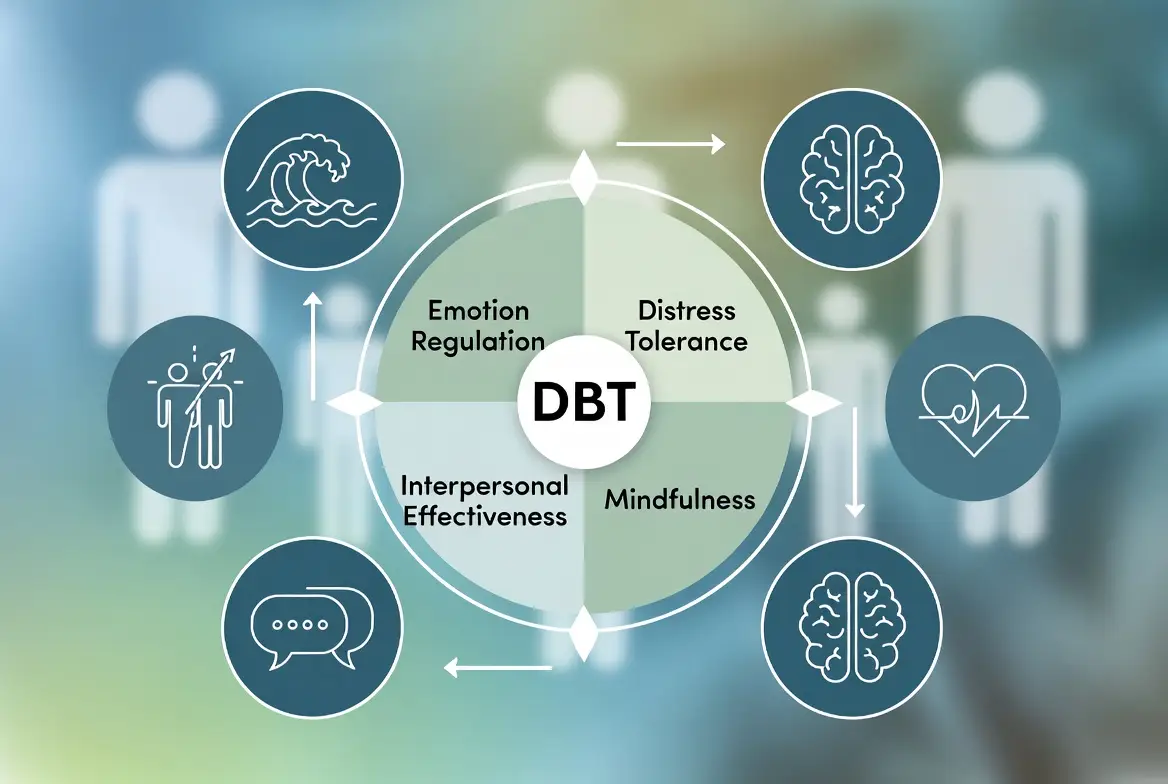
- Dialectical Behavior Therapy (DBT): While originally for other conditions, DBT’s focus on “distress tolerance” and “emotional regulation” is incredibly helpful for those experiencing rapid-cycling or mixed episodes.
- Group Therapy: Hearing from others who share your “internal weather” can be profoundly healing and reduces the isolation that bipolar disorder often creates.
Recommended Therapy for Bipolar Disorder: What Clinicians Actually Use

In a clinical setting, therapy interventions for bipolar disorder are rarely static. Your therapist will match the modality to your current mood state.
- During Depression: The focus is on CBT and Behavioral Activation. The goal is “gentle movement”—getting back to basic functioning without overwhelming the system.
- During Stability (Euthymia): This is the best time for IPSRT and FFT. When you are feeling well, you have the “bandwidth” to build routines and fix the relationship issues that occurred during the last episode.
- During hypomania, therapy shifts toward “limit-setting.” The therapist helps you stay grounded, maintain your medication schedule, and avoid impulsive financial or social decisions.
Medications Used Alongside Therapy
While this guide focuses on psychological interventions, it is impossible to discuss the recommended treatment for bipolar disorder without addressing medication. In 2026, the pharmacological approach has shifted toward “precision psychiatry,” where medications are chosen to minimize side effects while maximizing mood stability.
The Role of Mood Stabilizers
Mood stabilizers are the foundation of bipolar care. They work by leveling out the “waves” of neurotransmitter activity.
- Lithium: Still considered the gold standard for Bipolar I. It is uniquely effective at preventing mania and reducing the risk of suicide.
- Valproate (Depakote): Often used for “rapid cycling” or mixed episodes where symptoms of mania and depression occur simultaneously.
- Lamotrigine (Lamictal): The preferred treatment for bipolar 2. It is highly effective at preventing the “bottom” from falling out during depressive phases without triggering hypomania.
Atypical Antipsychotics
Modern antipsychotics such as Quetiapine (Seroquel), Lurasidone (Latuda), and Cariprazine (Vraylar) are now frequently used as first-line treatments. They are “atypical” because they influence both dopamine and serotonin receptors, helping to clear the “brain fog” of depression and the “static” of mania.
Why Therapy Improves Medication Outcomes
Many patients struggle with medication adherence due to side effects or the feeling that they “don’t need it” when they feel well. This is exactly where cognitive behavioral therapy for bipolar disorder excels. Therapy helps you process the grief of having a chronic illness and helps you realize that the medication isn’t “changing your personality”—it’s protecting your brain so your personality can shine through.
Lab Tests & Medical Monitoring in Bipolar Disorder
A critical but often overlooked part of the gold standard treatment for bipolar disorder is medical monitoring. Because bipolar disorder is a systemic biological condition, your physical health directly impacts your mental stability.
Why Labs Matter
There is currently no single blood test to diagnose bipolar disorder, but lab tests for bipolar disorder are essential for safety and optimization.
- Therapeutic Level Checks: If you are taking Lithium or Valproate, your doctor must check your blood levels to ensure the dose is high enough to work but low enough to avoid toxicity.
- Organ Function: Lithium requires monitoring of the thyroid and kidneys.
- Metabolic Panel: Some atypical antipsychotics can affect blood sugar and cholesterol. Regular labs ensure that while you are fixing your mood, you aren’t unintentionally hurting your metabolic health.
- The Vitamin D and B12 Connection: Clinicians often check for vitamin deficiencies that can mimic or worsen depressive symptoms.
Treatment Plans & Therapy PDFs Explained

When you enter a high-quality clinical program, your progress is usually tracked through a formal document. You may hear this referred to as a treatment plan for bipolar disorder pdf or an Individualized Treatment Plan (ITP).
What Is Inside a Formal Plan?
A professional treatment plan is more than just a list of goals; it is a roadmap for your recovery. It typically includes:
- Diagnostic Summary: Identifying whether you are Bipolar I, II, or Cyclothymic.
- Short-term Goals: (e.g., “Establish a consistent sleep-wake cycle within 30 minutes every day”).
- Long-term Goals: (e.g., “Return to full-time employment and maintain stability for six months”).
- Intervention Strategies: Explicitly listing what type of therapy is best for bipolar disorder for your specific case (e.g., “12 sessions of IPSRT”).
- Safety/Crisis Plan: A specialized section outlining who to call and what steps to take if you feel a “shift” starting.
What Not to Say to Someone With Bipolar Disorder
Managing a mood disorder is exhausting. The language used by friends and family can either be a bridge to recovery or a barrier to stigma. Understanding what not to say to someone with bipolar disorder is a key component of family-focused therapy for bipolar disorder.
Phrases to Avoid (and What to Say Instead)
- Don’t say: “Are you manic right now?” (This invalidates the person’s real emotions).
- Instead, say: “I’ve noticed you’ve been very energetic lately. How is your sleep going?”
- Don’t say: “You just need to think more positively.” (Bipolar is biological, not a lack of willpower).
- Instead, I say: “I can see you’re struggling with a low mood. I’m here to sit with you through this.”
- Don’t say: “I wish I had your energy when you’re ‘up’.” (This minimizes the danger and eventual “crash” of mania).
- Instead,d say: “I’m glad you’re feeling creative, but I want to make sure you’re also taking care of yourself.”
Can a Person Live a Normal Life With Bipolar Disorder?

This is perhaps the most frequent question in every therapist’s office. The short answer is: Yes, absolutely. However, the definition of “normal” might shift.
Redefining Stability
Can a person live a normal life with bipolar disorder? In 2026, we view “normal” not as the absence of a disorder, but as the mastery over it.
- Functional Recovery vs. Symptom Elimination: You may still have “echoes” of the disorder—a few days of low energy or a night of racing thoughts. But with the recommended treatment for bipolar, those echoes no longer have the power to destroy your life.
- The Role of Therapy in Longevity: Therapy provides the self-awareness needed to make long-term stability possible. Many people with bipolar disorder find that because they have to be so disciplined with their sleep, diet, and stress management, they actually end up healthier in the long run than people without the diagnosis.
Scholarly Research & Evidence-Based Support
When looking for the most effective treatment for bipolar disorder, it is essential to look at the data. Treatment for bipolar disorder, scholarly articles published in the mid-2020s have revolutionized our understanding of “neuro-progression.”
The “Kindling” Theory
Research shows that untreated mood episodes can actually “kindle” the brain, making it more sensitive to future episodes. This is why early intervention is so critical. A landmark 2025 meta-analysis confirmed that patients who engaged in cognitive behavioral therapy for bipolar disorder within the first year of diagnosis had a 40% lower rate of hospitalization over the following five years compared to those who received medication alone.
Neuroplasticity and Therapy
Scholarly evidence now suggests that specialized therapies like IPSRT don’t just change behavior; they support neuroplasticity. By stabilizing the circadian rhythm, therapy helps protect the hippocampus—the part of the brain responsible for memory and emotional regulation—from the toxic effects of high cortisol levels during mood episodes.
Frequently Asked Questions
What therapy is best for bipolar disorder?
The most effective approach is generally considered Interpersonal and Social Rhythm Therapy (IPSRT) combined with Cognitive Behavioral Therapy (CBT). While medication manages the chemical imbalance, these therapies provide the behavioral structure and cognitive tools necessary to prevent future relapses and manage daily stressors.
What type of therapy is best for bipolar disorder?
The “best” type depends on your primary struggle. For those with high-conflict home lives, Family-Focused Therapy (FFT) is superior. For those struggling with intense emotional outbursts or mixed episodes, Dialectical Behavior Therapy (DBT) is highly recommended. For those looking to master their daily routine and sleep, IPSRT is the gold standard.
What is the gold standard treatment for bipolar disorder?
The gold standard is the combined treatment model. This involves a synergy between mood-stabilizing medication (such as Lithium or Lamotrigine) and specialized psychotherapy. Clinical research consistently shows that individuals who use both medication and therapy have significantly better long-term outcomes than those using medication alone.
How to manage someone with bipolar disorder?
Managing a loved one with bipolar disorder involves a balance of support and boundaries. Key strategies include:
- Encouraging a strict sleep schedule.
- Attending Family-Focused Therapy to improve communication.
- Learning their “Relapse Signature” (early warning signs) so you can intervene gently before a crisis occurs.
- Avoiding judgmental language and focusing on biological stability.
Can a person live a normal life with bipolar disorder?
Yes. With modern recommended treatment for bipolar disorder, most individuals achieve functional recovery. “Normal” in this context means being able to sustain a career, raise a family, and engage in social life. While the disorder requires lifelong management, it does not prevent a person from reaching their highest personal and professional goals.
Conclusion
Finding the best therapy for bipolar disorder is a transformative step in a lifelong journey. As we have explored throughout this guide, stability is not a matter of luck; it is a matter of strategy. By integrating the biological safety net of medication with the psychological architecture of specialized therapies like CBT, IPSRT, and FFT, you can move from a state of “surviving” to “thriving.”
The recommended treatment for bipolar disorder in 2026 emphasizes the power of the individual. You are no longer a passive recipient of care, but an active manager of your own neurobiology. Whether you are managing Bipolar I or Bipolar II, the combination of professional guidance, data-driven treatment plans, and a disciplined lifestyle makes long-term health achievable.
Remember, recovery is not a straight line. There will be seasons of challenge, but with the right therapy modalities and a robust support system, you have the tools to navigate any emotional weather. Stability is possible, and a full, vibrant life is well within your reach.
Authoritative References
1. National Institute of Mental Health (NIMH)
2. American Psychiatric Association (APA)
3. Mayo Clinic: Bipolar Diagnosis & Treatment
Subscribe to Our Newsletter
Get mental health tips, updates, and resources delivered to your inbox.