What Therapy Types Help With Bipolar Mood Swings?

Navigating the highs and lows of bipolar disorder can feel like being caught in an emotional tidal wave. For those living with the condition, mood swings are more than just “ups and downs”; they are profound shifts in energy, thought patterns, and behavior that can disrupt every aspect of daily life. When these shifts occur, the most pressing question is often: What therapy types help with bipolar mood swings?
The journey toward stability is rarely a straight line, but modern clinical research in 2026 has made one thing clear: the most effective treatment for bipolar disorder is a multifaceted approach. While medication often acts as the chemical “floor” and “ceiling” to prevent extreme episodes, specialized psychotherapy provides the scaffolding. It teaches you how to recognize early warning signs, manage triggers, and rebuild a life that feels consistent and predictable.
There is no single “magic bullet” therapy that fits every individual. However, evidence-based recommended treatment for bipolar disorder typically involves a combination of mood stabilizers and structured psychological interventions. Whether you are dealing with the intense “highs” of Bipolar I or the lingering “lows” of Bipolar II, understanding your therapy options is the first step toward reclaiming control.
Understanding Bipolar Mood Swings and Treatment Goals
Bipolar mood swings are characterized by cycles of mania (or hypomania) and depression. In a manic state, a person might feel invincible, experience racing thoughts, and engage in impulsive behaviors. Conversely, a depressive episode can bring overwhelming sadness, fatigue, and a loss of interest in life. Some individuals even experience “mixed states,” where symptoms of both mania and depression collide simultaneously.
The treatment goals for bipolar disorder are tiered based on your current state:
- Acute Stabilization: The immediate goal during a severe episode is to ensure safety and reduce the intensity of symptoms.
- Maintenance and Prevention: Once stabilized, the focus shifts to preventing future relapses and extending the periods of “euthymia” (stable mood).
- Functional Recovery: Ultimately, the goal is to help you return to work, maintain relationships, and achieve a high quality of life.
Therapy is indispensable for the latter two goals. While medication targets the biological roots of the illness, therapy addresses the psychological and social factors that can trigger a relapse.
Recommended Treatment for Bipolar Disorder (Clinical Overview)
Clinical guidelines from organizations like the American Psychiatric Association (APA) and the National Institute for Health and Care Excellence (NICE) emphasize a “combination treatment model.” This means that for the vast majority of patients, recommended therapy for bipolar disorder should occur alongside pharmacological management.
Acute vs. Maintenance Treatment
In the acute phase of mania, the focus is almost entirely on medication (such as lithium or antipsychotics) to bring the brain’s “volume” down. However, during the maintenance phase, research consistently shows that patients who engage in psychotherapy have significantly lower relapse rates than those who rely on medication alone.
Individualized Care
Treatment must be tailored to the specific subtype (Bipolar I, Bipolar II, or Cyclothymic disorder) and the individual’s unique triggers. For some, the primary challenge is managing interpersonal conflict; for others, it is maintaining a strict sleep schedule. A high-quality recommended treatment for bipolar disorder will address these nuances directly.
What Type of Therapy Is Good for Bipolar Disorder?
When searching for what type of therapy is good for bipolar disorder, you will find several modalities that have stood the test of rigorous clinical trials. These are often referred to as “evidence-based” because they have been proven to work in real-world settings.
Best Therapy Modalities for Bipolar Disorder
- Cognitive Behavioral Therapy (CBT): Focuses on the relationship between thoughts, feelings, and behaviors.
- Interpersonal and Social Rhythm Therapy (IPSRT): Focuses on stabilizing daily routines and improving relationships.
- Family-Focused Therapy (FFT): Involves family members to improve communication and support systems.
- Dialectical Behavior Therapy (DBT): Originally for borderline personality disorder, it is increasingly used for bipolar to help with emotional regulation and distress tolerance.
It is important to remember that psychotherapy for bipolar disorder does not replace medication. Instead, it enhances it by increasing “medication adherence”—the likelihood that you will stay on your prescribed treatment—and providing the coping skills necessary to handle the stress that pills cannot fix.
1. Cognitive Behavioral Therapy (CBT) for Bipolar Disorder
Cognitive behavioral therapy for bipolar disorder is perhaps the most well-known and researched psychological intervention. The core philosophy of CBT is that while we cannot always control our circumstances or our biology, we can learn to identify and change the thought patterns that exacerbate mood swings.
Thought Patterns and Mood Regulation
During a depressive episode, CBT helps you identify “cognitive distortions”—such as “all-or-nothing thinking” or “catastrophizing”—that make the depression feel even more permanent and hopeless. In a hypomanic state, CBT can help you recognize overly optimistic or “grandiose” thoughts that might lead to risky decisions.
Relapse Prevention
One of the most powerful tools in CBT is the “Early Warning Sign” (EWS) analysis. You and your therapist work to identify the subtle changes that happen before a full episode hits. Does your sleep drop by two hours? Do you start cleaning the house at 3:00 AM? By catching these signs early, you can implement behavioral changes to “dampen” the impending swing.
2. Interpersonal and Social Rhythm Therapy (IPSRT)
Think of your brain like a finely tuned clock. For most people, if that clock ticks a little fast or slow, it’s no big deal. But with Bipolar disorder, the clock is incredibly sensitive. One late night or a skipped meal can send the whole system into a tailspin. This is where Interpersonal and Social Rhythm Therapy (IPSRT) steps in. It is essentially a manual for your biological rhythm.
The “Social Rhythm” Side
IPSRT is built on the “Social Zeitgeber” theory. This is a fancy way of saying our “body clock” (circadian rhythm) is pinned to our “social clock.” If your daily routine is chaotic, your mood will be too.
In therapy, you focus on five major anchors:
- Waking up: The time your eyes first open.
- First contact: The first person you interact with.
- Starting work/chores: When your day actually begins.
- Dinner: Your primary evening fuel.
- Bedtime: When you shut down.
By keeping these five events within a tight 45-minute window every single day—yes, even on weekends—you give your brain a sense of biological safety. You are telling your neurochemistry, “It’s okay, we know what’s coming next.”
The “Interpersonal” Side
Life happens. You might lose a job, start a new relationship, or have a big fight. For someone with Bipolar, these aren’t just “stresses”—they are potential triggers for a mood switch. IPSRT teaches you to navigate these relationship shifts without letting them blow up your physical routine.
Why It Works
You will likely use a tool called the Social Rhythm Metric (SRM). It’s a simple daily log. Over time, you’ll see the patterns. You might notice that when your “first contact” time drifts, a depressive “fog” follows three days later.
In short, IPSRT doesn’t just ask you how you feel. It looks at what you do. It turns “stability” from a vague hope into a measurable daily practice.
3. Family-Focused & Interpersonal Therapy
Bipolar disorder doesn’t happen in a vacuum. It lives in your living room, affects your partner, and shifts the vibe of your entire household. Because of this, treating the individual without involving their “ecosystem” is like fixing a car but ignoring the road it drives on.
Family-Focused Therapy (FFT): From Critics to Collaborators
FFT is built on a simple truth: a high-stress home can trigger a relapse. When family members don’t understand the biology of bipolar, they might mistake a depressive “low” for laziness or a manic “high” for selfishness.
In FFT, the family works with a therapist to:
- Lower “Expressed Emotion”: This means reducing criticism, hostility, or over-protectiveness that can unintentionally stress the patient.
- Spot the “Relapse Signature”: Often, a spouse or parent notices a mood shift before the person experiencing it does. FFT teaches them how to point this out without causing a fight.
- Enhance Communication: You learn to discuss the disorder as a medical reality, not a character flaw.
Interpersonal & Social Rhythm Therapy (IPSRT): Managing the “Social Clock”
While the “Social Rhythm” side (routines) is vital, the Interpersonal side is just as crucial. It focuses on how life events—like a breakup, a promotion, or a grief—disrupt your biological clock.
If you have a major conflict with a friend, it doesn’t just hurt your feelings; it ruins your sleep. Poor sleep then triggers a mood swing. IPSRT helps you resolve these interpersonal conflicts quickly to protect your “Social Zeitgebers” (your daily anchors).
Why This Combination Matters
By combining FFT and IPSRT, you aren’t just managing a list of symptoms; you are building a protective barrier. You stabilize your internal clock while your family stabilizes the environment around you. It turns a chaotic “tidal wave” into a manageable ripple.
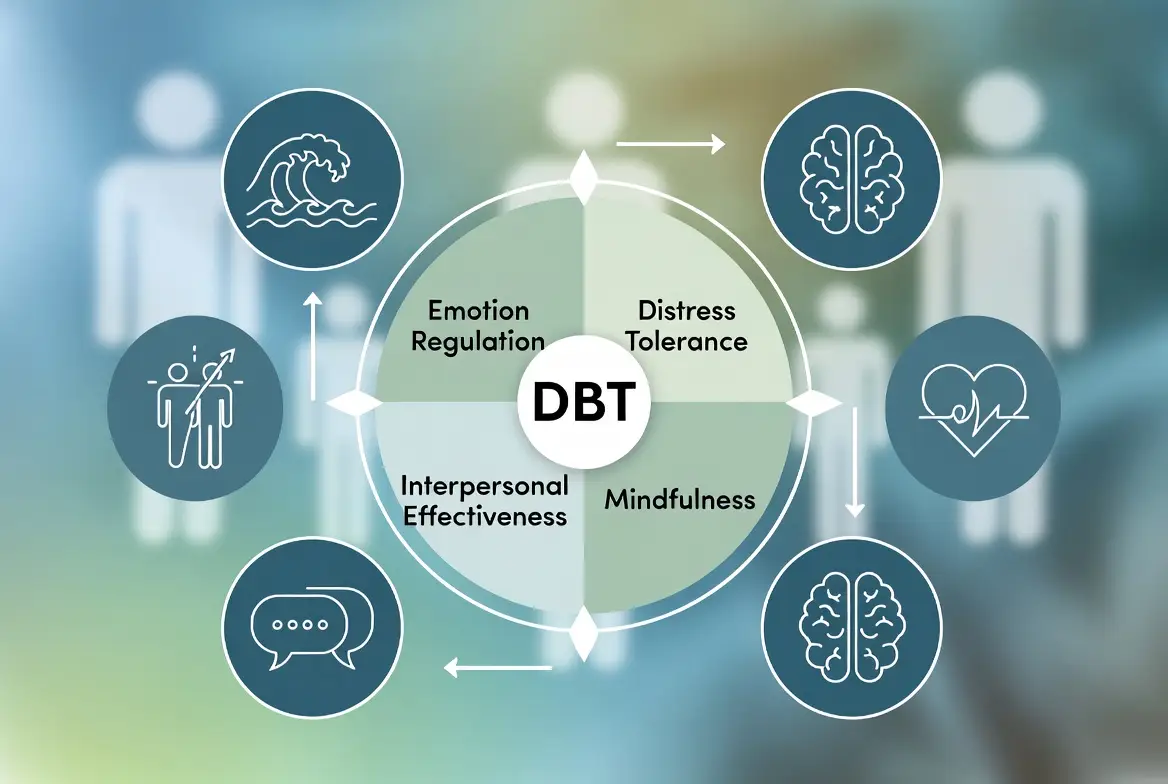
4. Dialectical Behavior Therapy (DBT)
DBT is like “Special Forces” training for your emotions. While other therapies look at routines or thoughts, DBT focuses on survival skills. It’s especially helpful for “mixed states”—that uncomfortable place where you feel the high energy of mania and the dark thoughts of depression at the same time.
The secret is in the word “Dialectical.” It means two opposite things can be true at once. You can accept exactly who you are right now, while simultaneously knowing you need to change your behavior to stay safe.
Here is how the four modules work in your daily life:
a. Mindfulness: The Observer Effect
Instead of being “hit” by a mood, you learn to step back. You notice a racing thought like a passing car rather than jumping in the driver’s seat. It creates a tiny gap between a feeling and an impulsive action.
b. Distress Tolerance: The Emergency Brake
When you’re manic and want to quit your job, or depressed and feeling hopeless, you use “Crisis Survival” skills. This involves techniques like the TIPP method (Temperature, Intense exercise, Paced breathing, and Paired muscle relaxation) to physically reset your nervous system.
c. Emotion Regulation: Turning the Dial
You learn “Opposite Action.” If depression tells you to stay in bed, you gently do the opposite and get up. If mania tells you to talk faster and do more, you intentionally slow your movements. You become the thermostat that controls the room, not just the thermometer that reads the heat.
d. Interpersonal Effectiveness: Relationship Repair
Bipolar episodes can leave a wake of broken bridges. DBT gives you a script to ask for what you need or set boundaries without burning your relationships down.
In short, DBT doesn’t just talk about the storm—it teaches you how to steer the ship while the waves are crashing.
Types of Supportive and Structured Bipolar Therapies
Beyond CBT, several other types of supportive bipolar therapy offer unique benefits depending on your life situation and specific symptoms.
Supportive Therapy and Counseling for Bipolar Disorder
What is the counseling for bipolar disorder? In many cases, it involves a blend of emotional support and practical problem-solving. Supportive therapy provides a safe space to process the grief of a diagnosis, the frustration of medication side effects, and the impact of the illness on one’s identity.
Therapy Techniques Used in Bipolar Disorder

Therapists use specific, actionable therapy techniques for bipolar disorder to help patients stay grounded. These are not just “talk” strategies; they are behavioral interventions.
- Mood Charting: Keeping a daily log of mood, sleep, and medication. This helps identify patterns that would otherwise go unnoticed.
- Behavioral Activation: During depression, small, manageable goals are set to break the cycle of withdrawal and inactivity.
- Sleep-Wake Stabilization: Creating a “sacred” sleep routine. For bipolar disorder, sleep is the most potent non-drug mood stabilizer available.
- Crisis Planning: Creating a “treatment plan for bipolar disorder pdf” or digital document that outlines what to do when you are in a crisis, including who to call and which medications to adjust (under doctor supervision).
Coping Skills for Bipolar People (Learned in Therapy)
While therapy sessions provide a space for deep work, the true test of recovery happens in the “real world.” What are the coping skills for bipolar people that make the difference between a relapse and stability? These skills are often the practical takeaway from structured therapy interventions.
- Emotional Regulation: Techniques such as “opposite action” (doing the opposite of what a depressive or manic urge dictates) help gain distance from intense emotions.
- Stress Reduction and Mindfulness: High levels of cortisol can trigger mood switches. Mindfulness teaches you to observe a racing thought without necessarily “boarding the train” and following it into impulsive action.
- The “Two-Day Rule”: A common technique for managing hypomania. If you have a “brilliant” idea to quit your job or spend a large sum of money, you commit to waiting 48 hours and discussing it with a “stability partner” before acting.
- Proactive Crisis Planning: This involves creating a detailed document while you are stable. It outlines exactly how you want to be treated if you lose insight during a manic episode, including which hospital you prefer and who has power of attorney.
Bipolar I vs. Bipolar II — Treatment Differences
It is a common misconception that Bipolar II is “Bipolar Lite.” In reality, the two subtypes require distinct strategies, particularly when it comes to bipolar 2 treatment options.
Bipolar 1 Treatment Focus
In Bipolar I, the primary clinical danger is mania. Because mania can involve psychosis and total loss of judgment, the most effective treatment for bipolar disorder type 1 focuses on containment. Therapy often focuses heavily on medication adherence and recognizing the “euphoric” warning signs that lead to hospitalization.
Bipolar 2 Treatment Options and Best Practices
For those seeking the best treatment for bipolar 2, the focus shifts to the depressive pole. People with Bipolar II spend significantly more time in debilitating depression than in hypomania.
- Depression Management: Therapy must be more intensive regarding “leaden paralysis” and chronic low self-esteem.
- Hypomania Awareness: Because hypomania can feel productive or even “normal,” therapy helps the individual identify the subtle irritability or sleep loss that indicates an upward swing.
How to Treat Bipolar Mood Swings (Therapy + Medication)
The most sustainable way to treat bipolar mood swings is to view the condition as a three-legged stool: medication, therapy, and routine. If any one leg is missing, the structure is prone to collapse.
Medication Stabilizes Biology
Medication acts as the “thermostat” for the brain. It prevents the neurotransmitters—dopamine, serotonin, and norepinephrine—from fluctuating wildly. Without this biological floor, even the best therapy techniques may feel impossible to implement.
Therapy Stabilizes Behavior
If medication fixes the “hardware,” therapy fixes the “software.” It teaches you how to navigate the psychological fallout of having a chronic illness. It helps rebuild self-esteem, repair relationships damaged during episodes, and provides the “manual” for how to live a stable life.
Routine Supports Both
No pill or therapy session can overcome the damage of a chaotic lifestyle. Stability is built on the foundation of consistent sleep, regular meals, and a balanced workload.
What Are the Top 10 Medications for Bipolar Disorder?
While only a psychiatrist can prescribe, it is helpful for patients to be informed about what are the top 10 medications for bipolar disorder. These are typically categorized into mood stabilizers and atypical antipsychotics.
| Category | Common Examples | Primary Role |
| Mood Stabilizers | Lithium, Valproate, Lamotrigine | Prevents “highs” and “lows”; the gold standard. |
| Atypical Antipsychotics | Quetiapine, Aripiprazole, Risperidone | Treats acute mania and bipolar depression. |
| Atypical Antipsychotics (Newer) | Lurasidone, Cariprazine | Specifically targeted at bipolar depression. |
| Anticonvulsants | Carbamazepine, Oxcarbazepine | Used when traditional stabilizers aren’t effective. |
Frequently Asked Questions
What is the “best” therapy for bipolar disorder?
While there is no single “best,” the consensus among researchers is that Interpersonal and Social Rhythm Therapy (IPSRT) combined with CBT offers the most robust protection against relapse because it addresses both biological rhythms and psychological thought patterns.
Can I treat bipolar mood swings with therapy alone?
Generally, no. Bipolar disorder is a biological condition involving neurotransmitter dysregulation. While therapy is essential for managing behavior and stress, medication is usually required to provide the biological stability that allows therapy to work.
How long does it take for therapy to help?
Coping skills can be learned in a few sessions, but the goal of therapy for bipolar disorder is long-term management. Most structured programs, like CBT for Bipolar, last between 12 and 20 sessions, but many patients benefit from “maintenance” therapy once or twice a month for years.
Does Bipolar 2 require different therapy than Bipolar 1?
The type of therapy (CBT, IPSRT) is often the same, but the focus is different. Bipolar 2 therapy focuses more on lifting chronic depression and identifying “hypomania” (which can be harder to spot than full mania).
What is the role of the family in bipolar therapy?
Family members often act as the “early warning system.” Family-Focused Therapy teaches them how to provide support without being overbearing and how to communicate effectively during high-stress episodes.
Conclusion
Mastering bipolar disorder is a transition from being a passenger to being the pilot of your own neurochemistry. As this 2026 guide has detailed, the most effective treatment for bipolar disorder is never found in a single intervention. Instead, it is the result of a “synergistic” strategy: medication provides the chemical safety net, psychotherapy builds the mental resilience, and routine stabilizes the biological clock.
The data is clear—bipolar disorder is a lifelong journey, but it does not have to be a life of perpetual crisis. By integrating recommended therapy for bipolar disorder, like CBT or IPSRT, with a dedicated medical team, you move beyond mere symptom management toward functional recovery. This means returning to the relationships, careers, and hobbies that define who you are, rather than who the disorder makes you feel like you are.
Authoritative References
- American Psychiatric Association (APA): APA Website
- National Institute of Mental Health (NIMH): NIMH Website
- National Institute for Health and Care Excellence (NICE): NICE Website
- Journal of Clinical Psychiatry: JCP Website
- Depression and Bipolar Support Alliance (DBSA): DBSA Website
Subscribe to Our Newsletter
Get mental health tips, updates, and resources delivered to your inbox.