New Treatments for Borderline Personality Disorder and Evidence-Based
For decades, a diagnosis of Borderline Personality Disorder (BPD) was often met with a heavy sense of clinical nihilism. Many patients—and even some healthcare providers—believed the condition was a lifelong sentence of emotional chaos that simply couldn’t be fixed. This outdated myth has been thoroughly dismantled by modern science.
Today, if you are asking, “Is borderline personality disorder treatable?” the answer from the clinical community is a resounding yes. In fact, BPD is now considered one of the most treatable personality disorders. We have moved from a period of “managing the crisis” to a new era of “functional recovery.” Modern care doesn’t just aim to stop self-destructive behaviors; it aims to build a “life worth living,” a phrase popularized by the creators of the best treatment for borderline personality disorder: Dialectical Behavior Therapy (DBT).
In this article, we will explore the new treatments for borderline personality disorder emerging in 2026, the rigorous clinical guidelines that ensure patient safety, and the specialized therapies that have turned BPD from a “hopeless” label into a roadmap for profound personal growth. Whether you are a patient, a family member, or a clinician, understanding these evidence-based options is the first step toward lasting stability.
Is Borderline Personality Disorder Treatable?
The short, direct answer is: Yes, BPD is highly treatable. Longitudinal research, such as the famous McLean Study of Adult Development, has shown that after ten years of treatment, nearly 86% of patients with BPD reach sustained remission.
Symptom Remission vs. Functional Recovery
It is important to understand what “treatable” means in a clinical context. There is a distinction between symptom remission and functional recovery:
- Symptom Remission: This means you no longer meet the diagnostic criteria for BPD. Most patients reach this stage relatively quickly (within 1 to 3 years) with consistent, specialized therapy.
- Functional Recovery: This refers to the ability to hold a steady job, maintain healthy long-term relationships, and feel a consistent sense of self. This process often takes longer, but it is the ultimate goal of evidence-based treatments for BPD.
Unlike some other mental health conditions, BPD traits tend to “mellow” with age, and when paired with targeted interventions, the prognosis is exceptionally positive. The “new calculus” of BPD care in 2026 focuses on early intervention—identifying traits in adolescence to prevent the years of suffering that often precede an adult diagnosis.
What Triggers a Person With Borderline Personality Disorder?
Understanding the “why” behind the emotional storms is central to modern treatment. If we don’t know what triggers a person with borderline personality disorder, we cannot apply the right skills to manage the reaction.
Common Emotional and Environmental Triggers
Most BPD triggers are interpersonal. They often center around the “biosocial” vulnerability of the individual—a high sensitivity to rejection combined with an environment that may not have taught them how to regulate that sensitivity.
- Fear of Abandonment: A late text message, a partner going out with friends, or a therapist going on vacation can trigger an intense “fight or flight” response.
- Perceived Criticism: Because of a “negativity bias,” a neutral comment might be interpreted as a devastating personal attack.
- Identity Shifts: Stressful life changes (like starting a new job) can trigger a loss of self-identity, leading to “splitting” or impulsive behavior.
Trigger awareness is the cornerstone of borderline personality disorder therapy techniques. By identifying these patterns, patients learn that their reactions—while intense—are predictable and, therefore, manageable.
Borderline Personality Disorder Treatment Guidelines
To ensure that patients receive high-quality care, several major health organizations have established a borderline personality disorder treatment guideline. These frameworks prevent “treatment by trial and error” and ensure clinicians follow the best available science.
APA and NICE Frameworks
The APA (American Psychiatric Association) updated its guidelines in 2024–2025, emphasizing a shift toward “person-centered” care. Similarly, the NICE (National Institute for Health and Care Excellence) guidelines in the UK provide a rigorous standard for NHS care.
- Psychotherapy as First-Line: Every major guideline states that specialized talk therapy is the primary treatment.
- Medication as Adjunct: Medication should never be the sole treatment for BPD. It is used only to support the work done in therapy.
- Diagnosis Disclosure: Guidelines now strongly encourage “diagnostic transparency”—telling the patient they have BPD and providing education about it, which has been shown to reduce stigma and improve outcomes.
What Is the Most Effective Treatment for Borderline Personality Disorder?
When families ask, “What is the most effective treatment for borderline personality disorder?” the answer is Structured Psychotherapy.
There is no “miracle pill” for personality. Because BPD is a disorder of emotional regulation and interpersonal patterns, it requires a treatment that “rewires” how the brain processes these experiences. According to the evidence hierarchy:
- Gold Standard: Dialectical Behavior Therapy (DBT) remains the most researched and effective intervention, particularly for high-risk behaviors like self-harm.
- High Effectiveness: Mentalization-Based Therapy (MBT) and Schema Therapy have shown nearly equal success rates, especially for improving long-term relationship stability.
The “best” treatment is often the one that the patient can access consistently, and that matches their specific symptom profile (e.g., DBT for crisis management vs. Schema Therapy for deep-seated identity issues).
Dialectical Behavior Therapy (DBT): Gold-Standard Treatment

Developed by Dr. Marsha Linehan, DBT interventions for borderline personality disorder changed the landscape of psychiatry. DBT is based on a “dialectical” philosophy—the idea that two seemingly opposite things can be true at once: Acceptance and Change.
The Four Pillars of DBT
- Mindfulness: Learning to be present in the moment without judgment.
- Distress Tolerance: Getting through a crisis without making it worse (e.g., “TIPP” skills to change body chemistry).
- Emotion Regulation: Learning to “tame” intense emotions before they become overwhelming.
- Interpersonal Effectiveness: Learning how to say “no” or ask for what you need while keeping relationships healthy.
DBT is not just “talking.” It involves weekly individual therapy, a group skills-training class, and “phone coaching” where the therapist helps the patient apply skills in real-time crises. This multi-layered approach is why it remains the best treatment for borderline personality disorder.
Schema Therapy for Borderline Personality Disorder
While DBT focuses on “extinguishing the fire” of current symptoms, schema therapy for borderline personality disorder focuses on the “architectural flaws” that keep the fire from starting. It is an integrative therapy that combines elements of CBT, psychoanalysis, and attachment theory.
Core Schemas and Modes
Schema therapy suggests that BPD is the result of “Early Maladaptive Schemas”—deep-seated patterns of thinking formed when a child’s basic emotional needs (safety, autonomy, limits) were not met. In BPD, these schemas manifest as “Modes”:
- The Abandoned/Vulnerable Child: The part of the patient that feels small, terrified, and alone.
- The Angry Child: The part that lashes out when needs aren’t met.
- The Punitive Parent: The internal voice that tells the patient they are “bad” or “worthless.”
- The Healthy Adult: The part that the therapist works to grow, which can eventually soothe the child’s modes and silence the punitive parent.
Research in 2025–2026 has shown that schema therapy is particularly effective for “functional recovery”—helping patients move past just surviving to actually thriving in their identities and careers.
Other Evidence-Based Therapies for BPD
Beyond DBT and Schema Therapy, several other evidence-based treatments for BPD are vital for a personalized recovery plan.
- Mentalization-Based Therapy (MBT): This focuses on “thinking about thinking.” It helps patients realize that their internal feelings aren’t always facts and that other people have their own separate, complex internal lives.
- Transference-Focused Psychotherapy (TFP): This uses the relationship between the patient and the therapist as a “laboratory.” By observing how the patient reacts to the therapist, they can identify and fix distorted interpersonal patterns in real-time.
- STEPPS: A 20-week group program often used as an adjunct to individual therapy, focusing on “systems training” for emotional predictability.
Borderline Personality Disorder Treatment Plan: What It Includes
A professional treatment plan for borderline personality disorder is a living document. It shouldn’t be a “DIY” list but a structured agreement between a patient and their clinical team.
Essential Components
- Comprehensive Assessment: Identifying co-occurring conditions like PTSD, depression, or substance use.
- Crisis Component: A specific “Safety Plan” for what to do during suicidal ideation or self-harm urges.
- Target Hierarchy: DBT, for example, prioritizes life-threatening behaviors first, then therapy-interfering behaviors, then quality-of-life issues.
- Family Psychoeducation: Including family members is now a standard borderline personality disorder treatment guideline to help them understand triggers and reduce household stress.
Medication for Borderline Personality Disorder: What Helps and What Doesn’t
One of the most common questions from patients is: “What is the happy pill for BPD?“
Debunking the “Happy Pill” Myth
As of 2026, there is no FDA-approved medication specifically for BPD. There is no “happy pill” that can change a personality. Antidepressants, while often prescribed, have shown only modest effects on BPD itself, though they help significantly if the patient has co-occurring clinical depression.
Targeted Symptom Management
- Mood Stabilizers (e.g., Lamotrigine): These can help with “affective instability”—the rapid, jagged mood swings that feel like an emotional roller coaster.
- Atypical Antipsychotics (e.g., Quetiapine, Aripiprazole): In low doses, these are effective for “cognitive-perceptual” symptoms like paranoia or intense anger.
- Memantine (Namenda): An emerging area of research is the use of memantine for borderline personality disorder. Originally used for Alzheimer’s, new trials (NCT02097706) are investigating its role in reducing glutamate-related impulsivity and cognitive “fog.”
How to Stop Splitting in BPD
“Splitting” is a defense mechanism where a person views things as all-good or all-bad (black-and-white thinking). Learning how to stop splitting BPD is a primary goal of therapy.
Evidence-Based Techniques
- “Both-And” Thinking: Replacing “Either/Or” with “Both/And.” Example: “I am angry with my partner, and they are still a good person who loves me.”
- Reality Testing: Asking for evidence. “Do I have proof they hate me, or am I reacting to a feeling of being ignored?”
- Mindful Pausing: Splitting is usually an impulsive “snap.” Creating even a 5-minute buffer between the feeling and the reaction can allow the “Healthy Adult” mode to take over.
Does Having BPD Qualify for Disability?
For many, BPD is a “hidden disability.” If you are wondering, does having BPD qualify for disability? The answer depends on your “functional impairment.”
In the US, the Social Security Administration (SSA) lists BPD under Listing 12.08. To qualify for SSDI or SSI, you must prove that your BPD creates an “extreme limitation” in your ability to:
- Understand and apply information.
- Interact with others.
- Concentrate and maintain pace.
- Adapt or manage oneself.
Because BPD symptoms can be erratic, consistent medical documentation and a long-term treatment history are the most important factors for a successful disability claim.
New and Emerging Treatments for Borderline Personality Disorder

As we move into 2026, the “landscape of hope” for BPD has expanded significantly. Researchers are no longer just looking at how to reduce symptoms, but how to change the brain’s underlying architecture.
1. Neuromodulation and Brain Stimulation
One of the most exciting new treatments for borderline personality disorder involves non-invasive brain stimulation.
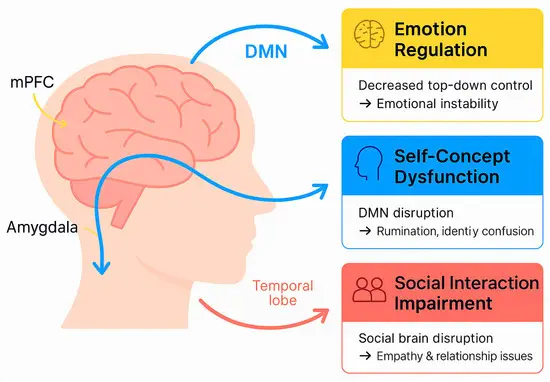
- Repetitive Transcranial Magnetic Stimulation (rTMS): Clinical trials in late 2025 and 2026 (such as those at UCLA) are exploring how magnetic pulses can “calm” the overactive amygdala (the brain’s fear center) and “strengthen” the prefrontal cortex (the brain’s brake system).
- tDCS (Transcranial Direct Current Stimulation): This portable technology is being studied as a way to help patients regulate their emotions in real-time by providing a mild electrical current to specific brain regions associated with impulse control.
2. Technology-Assisted DBT and Digital Therapeutics
To solve the problem of long waiting lists, technology-assisted DBT has become a reality.
- DBT Apps: These aren’t just trackers; they are interactive “coaches” that use AI to suggest specific distress tolerance skills based on a patient’s heart rate or typing speed.
- Virtual Reality (VR) Exposure: VR is being used to help patients practice “Interpersonal Effectiveness” skills in a safe, simulated environment—such as practicing a difficult conversation with a “boss” or “partner” before doing it in real life.
3. Ketamine and Glutamate Research
While traditionally used for treatment-resistant depression, ketamine for BPD is a major research frontier in 2026. Studies suggest that ketamine’s ability to promote “synaptic plasticity”—essentially helping the brain grow new connections—may help patients “unlearn” traumatic response patterns more quickly when combined with therapy.
4. Internal Family Systems (IFS) for BPD
While DBT is the “gold standard,” Internal Family Systems (IFS) is a rising star in 2026. This therapy views the BPD experience as a collection of “parts”—such as a “Protector” part that uses anger to keep others away, or an “Exiled” part that carries deep trauma. By helping the “Self” lead these parts, patients often report a deeper sense of internal harmony than behavioral skills alone can provide.
“I Cured My Borderline Personality Disorder”: What Recovery Really Means
You will often see people online stating, “I cured my borderline personality disorder.” In the psychiatric community, we use the term “recovery” or “remission” rather than “cure.”
Is There a Cure?
Personality is not a virus that can be eliminated; it is the way you are “wired” to interact with the world. However, you can reach a point where you:
- No longer meet the 9 criteria: You may still feel things deeply, but you no longer self-harm, split, or have unstable relationships.
- Achieve “Symptomatic Remission”: The symptoms are present but no longer control your life.
Most people who say they are “cured” mean that BPD has moved from being the “pilot” of their life to a “passenger” that they know how to manage.
Best Practices for Long-Term Management and Relapse Prevention
Recovery from BPD is a marathon, not a sprint. The best treatment for borderline personality disorder includes a robust maintenance plan.
- Maintenance Therapy: Transitioning from twice-weekly therapy to once a month or “as needed.”
- Skills Reinforcement: Continuing to use DBT “Diary Cards” even when things are going well.
- Support Systems: Peer support groups (like Emotions Matter or NEABPD) provide a space where you don’t have to explain your symptoms—everyone already understands.
- Life Transitions: Being extra vigilant during big changes (new job, moving, breakups), as these are the times when old BPD “parts” are most likely to resurface.
Frequently Asked Questions
Is borderline personality disorder treatable?
Yes. With evidence-based therapy, over 80% of patients reach diagnostic remission within 10 years, and many see significant improvement within the first year.
What is the most effective treatment for BPD?
Dialectical Behavior Therapy (DBT) is the gold standard, though Mentalization-Based Therapy (MBT) and Schema Therapy are also highly effective.
What is the “happy pill” for BPD?
There is no “happy pill.” Medication is used only to manage specific symptoms like anxiety or mood swings, while therapy does the heavy lifting of changing personality patterns.
How to stop splitting in BPD?
Use “Both/And” thinking, practice mindfulness to catch the “black-and-white” thought early, and wait 24 hours before acting on an intense feeling about someone.
Does BPD qualify as a disability?
Yes, if it causes significant “functional impairment” that prevents you from working or managing daily life. It requires extensive medical documentation for approval.
Are new treatments available for BPD?
Yes. 2026 has seen the rise of brain stimulation (rTMS), ketamine-assisted therapy, and digital DBT tools.
Conclusion
The most important thing to know about new treatments for borderline personality disorder is that they work. We are no longer in an era where BPD is a “mystery” or a “dead end.” It is a well-understood condition with a clear clinical pathway.
Recovery doesn’t mean you will never feel intense emotions again. It means you will have the tools to navigate those emotions without losing yourself. It means your relationships will stop being “stormy” and start being “stable.” With the right borderline personality disorder treatment plan, a life of purpose, connection, and joy is not just a dream—it is the expected outcome.
Authoritative References
1. American Psychiatric Association (APA) – Clinical Practice Guidelines
2. National Institute of Mental Health (NIMH) – BPD Research Portal
3. The Cochrane Library – Psychological Therapies for BPD
4. National Education Alliance for BPD (NEABPD)
5. ClinicalTrials.gov – Current BPD Treatment Research
Subscribe to Our Newsletter
Get mental health tips, updates, and resources delivered to your inbox.