What Causes Borderline Personality Disorder? Understanding the Root Causes of BPD

Borderline Personality Disorder (BPD) is often described by those who live with it as having “emotional third-degree burns.” For people with BPD, the world feels sharper, louder, and more painful than it does for others. But where does this intense sensitivity come from?
If you are asking what causes borderline personality disorder, you are not alone. For decades, the mental health community has sought to unravel the complex web of genetics, biology, and environment that leads to this diagnosis. Understanding the root causes is not just an academic exercise; it is a vital step toward reducing stigma and finding the right path to recovery.
What Is Borderline Personality Disorder?
Before diving into the “why,” we must understand the “what.”
Borderline Personality Disorder is a mental health condition characterized by a pervasive pattern of instability in emotions, self-image, and relationships.
The signs of borderline personality disorder usually emerge in late adolescence or early adulthood. Common symptoms of borderline personality disorder include frantic efforts to avoid abandonment, impulsive behaviors, and chronic feelings of emptiness.
Understanding borderline personality disorder, what causes it? It is crucial because it shifts the narrative from “bad behavior” to “biological and psychological injury.” When we recognize BPD as a legitimate health condition rooted in specific causes, treatment becomes about healing and skill-building rather than blame.
Are People Born With BPD or Does It Develop Over Time?
A common question for families is: Are people born with BPD? The short answer is that people are not born with the disorder itself, but they are born with the biological temperament that makes them vulnerable to it.
Current research suggests that BPD is a developmental disorder. This means it is the result of a “perfect storm” where a child’s natural, inherited emotional sensitivity meets an environment that cannot support or validate those intense feelings.
Nature vs. Nurture
In the debate of nature versus nurture, BPD is a classic example of both.
- Nature: Provides the “high-reactive” nervous system.
- Nurture: Provides the experiences (or lack thereof) that either soothe the nervous system or aggravate it.
Because personality is something that forms over time, BPD is not considered a congenital condition present at birth. Instead, it is the outcome of how a sensitive child learns—or fails to learn—to regulate their emotions throughout their formative years.
What Are the Root Causes of Borderline Personality Disorder?
Psychologists generally point to three primary “pillars” when explaining what causes a borderline personality disorder. This is often referred to as the Biosocial Model, developed by Dr. Marsha Linehan.
1. Biological Vulnerability
Some individuals are simply born with “thinner skin.” Their emotional baseline is higher, their reactions are more intense, and it takes them much longer to return to a state of calm after being upset.
2. Psychological Development
As a child grows, they must learn “mentalization”—the ability to understand their own mental states and those of others. Disruptions in this development, often due to attachment issues, can lead to the identity confusion seen in BPD.
3. Environmental Stressors
This includes the external world: family dynamics, school experiences, and traumatic events. What causes someone to have borderline personality disorder is often an “invalidating environment” where the child is told their feelings are wrong, dramatic, or unnecessary.
Childhood Causes of Borderline Personality Disorder
The environment a child grows up in acts as the soil for their developing personality. When that soil is unstable, BPD symptoms are more likely to take root.
Emotional Neglect
Neglect is often “the trauma of what didn’t happen.” When a child’s emotional needs are consistently ignored, they fail to develop a sense of self-worth. They may grow up feeling invisible, leading to the “chronic emptiness” and “identity disturbance” found in BPD.
Inconsistent Caregiving
If a parent is warm and loving one day but cold and frightening the next, the child develops “disorganized attachment.” They learn that the person they rely on for safety is also a source of fear. This creates a blueprint for the “I hate you, don’t leave me” relationship patterns in adulthood.
Invalidating Environments
An invalidating environment is one where a child’s inner experiences are dismissed, punished, or mocked. If a sensitive child cries and is told “stop being a baby” or “it’s not that big of a deal,” they learn to distrust their own emotions. Eventually, they may resort to extreme behaviors (like self-harm) just to feel heard or to communicate the depth of their internal pain.
What Causes Quiet Borderline Personality Disorder?
While “Classic” BPD is often identified by outward explosions of anger, the causes of quiet borderline personality disorder lead to a very different presentation. This subtype is characterized by “acting in” rather than “acting out.”
Internalized Coping Styles
Quiet BPD often develops in children who learned that expressing anger or distress was dangerous or socially unacceptable. If a child was punished for crying or shamed for being angry, they may have developed a “mask” of compliance while their emotional turmoil raged internally.
Suppressed Anger and Self-Blame
Unlike the “BPD rage” directed at others, those with Quiet BPD turn that intensity toward themselves. They are often their own harshest critics, experiencing deep shame and guilt. The root cause is frequently a high level of perfectionism used as a defense mechanism—if they are “perfect,” they believe they can prevent the abandonment they so deeply fear.
What Causes BPD in Females?
Statistics often show higher diagnosis rates for women, leading many to ask what causes BPD in females. While the core biological and environmental factors remain the same, there are unique nuances to the female experience of the disorder.
Gendered Trauma Exposure
Women and girls are statistically more likely to experience certain types of childhood trauma, specifically sexual abuse and relational bullying, both of which are high-risk factors for developing BPD.
Hormonal Influences
Research suggests that fluctuations in estrogen and progesterone during the menstrual cycle can exacerbate BPD symptoms. Some women experience a significant worsening of emotional instability and rejection sensitivity during the luteal phase (the week before their period), a phenomenon sometimes called “perimenstrual exacerbation.”
Social Conditioning
Society often socializes women to be “relationship-focused.” For a person with a biological vulnerability to BPD, this cultural pressure can intensify the fear of abandonment, making relationship stability feel like the only measure of self-worth.
Trauma and Abuse as Major Causes of BPD
While not everyone with BPD has a history of trauma, a significant majority do. Research indicates that up to 70-80% of individuals diagnosed with BPD report childhood maltreatment.
Childhood Trauma
Trauma acts as a powerful catalyst for what causes borderline personality disorder symptoms. When a child experiences physical, sexual, or emotional abuse, their brain stays in a constant state of “fight or flight.” This prevents the development of the prefrontal cortex—the part of the brain responsible for logical thinking and emotional “brakes.”
Attachment Disruption
Losing a primary caregiver early in life—through death, divorce, or incarceration—can leave a permanent scar. The intense fear of abandonment in BPD is often a literal echo of a time when the person actually was abandoned or neglected when they were most vulnerable.
Biological and Genetic Factors in Borderline Personality Disorder
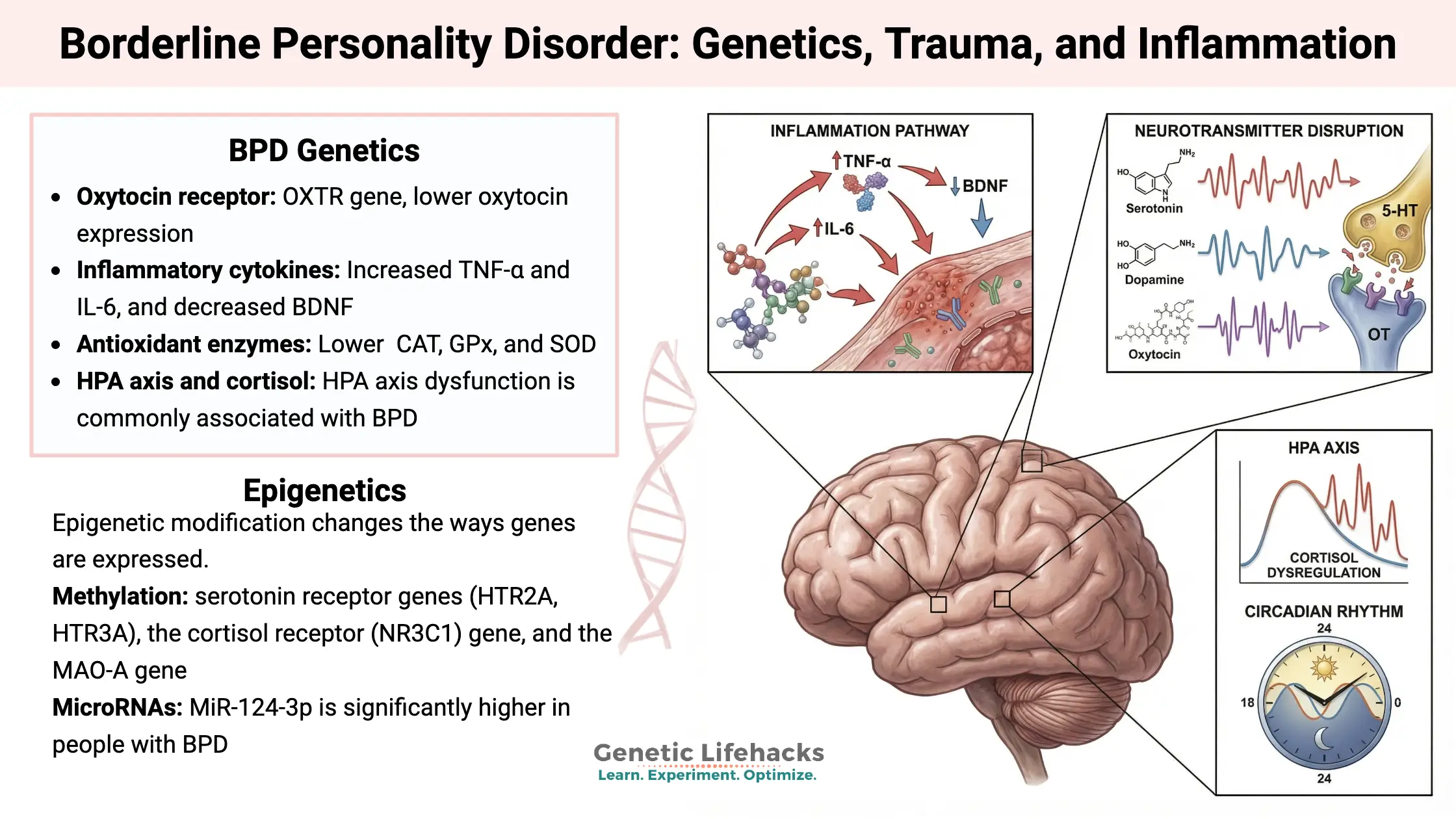
Science has shown that the factors that contribute to the development of borderline personality disorder are deeply etched into our biology.
Genetics and Family History
BPD is highly heritable. Studies of twins show that if one identical twin has BPD, the other is significantly more likely to have it than in fraternal twins. If you have a first-degree relative with BPD, you are roughly five times more likely to develop the disorder.
Brain Structure and Function
Neuroimaging has revealed distinct differences in the BPD brain:
- The Amygdala: This “alarm system” is hyper-reactive, causing intense fear and anger over small triggers.
- The Hippocampus: Often smaller in those with BPD, affecting how they process stress and memories.
- The Prefrontal Cortex: This area is often underactive, making it incredibly difficult for the person to “think through” an emotional impulse before acting on it.
What Triggers Borderline Personality Disorder Symptoms?
Understanding what triggers a person with borderline personality disorder is key to managing the condition. A trigger is a “spark” that sets off the “explosive” emotional reaction.
- Perceived Rejection: A delayed text message, a neutral facial expression, or a friend hanging out with someone else can trigger a “spiral” of panic.
- Fear of Abandonment: Situations like a partner going on a business trip or a therapist going on vacation can feel like a life-threatening loss.
- Relationship Instability: Arguments or even small disagreements can trigger “splitting,” where the person suddenly sees their loved one as a “villain.”
- Reminders of Past Trauma: Certain smells, locations, or phrases can subconsciously trigger the brain’s “alarm system,” even if the person isn’t consciously remembering the trauma.
What Causes Borderline Personality Disorder Symptoms to Worsen?
Even after a diagnosis, certain factors can cause borderline personality disorder symptoms to flare up or become more severe.
- Chronic Stress: High-pressure jobs or unstable living situations drain the limited “emotional reserves” a person with BPD has.
- Substance Use: Alcohol and drugs are often used to “numb” the pain, but they actually weaken the prefrontal cortex, leading to even more impulsivity and emotional “crashes.”
- Lack of Sleep: Sleep deprivation is a major trigger for emotional dysregulation, making it nearly impossible to use coping skills like mindfulness.
- Isolation: When a person with BPD pulls away from their support system, their “internal critic” grows louder, often leading to increased self-harm or suicidal ideation.
Can People With BPD Seem Normal?
One of the most confusing aspects for friends and family is the question: Can people with BPD seem normal? The answer is a resounding yes. This is often referred to as “masking” or “high-functioning BPD.”
Many individuals with BPD are exceptionally high achievers. They may be successful doctors, artists, or parents who appear perfectly composed in public. However, they are often “white-knuckling” their way through the day, experiencing intense internal agony that they only release when they are alone or with their most trusted person. This “hidden” nature of the disorder is why many go undiagnosed for years.
What Are the 9 Traits of Borderline Personality Disorder?
The DSM-5 outlines 9 traits of borderline personality disorder. To receive a diagnosis, a person generally must consistently display at least five of these:
- Fear of Abandonment: Frantic efforts to avoid real or imagined being left alone.
- Unstable Relationships: A pattern of “idealizing” then “devaluing” others.
- Identity Disturbance: Feeling like you don’t know who you are or what you believe in.
- Impulsivity: Self-damaging behaviors (spending, sex, substance use, etc.).
- Self-Harm: Recurrent suicidal threats, gestures, or self-mutilation.
- Emotional Instability: Intense “mood crashes” that last hours to a few days.
- Chronic Emptiness: Feeling “hollow” or like there is a void inside.
- Explosive Anger: Difficulty controlling temper or frequent physical fights.
- Dissociation/Paranoia: Feeling “spaced out” or suspicious under high stress.
How BPD Differs From Bipolar Disorder
Misdiagnosis is common because both involve mood swings. However, the causes of bipolar disorder are primarily biological and chemical, involving distinct “episodes” of mania and depression that can last weeks.
BPD mood swings are reactive. They are almost always triggered by an interpersonal event (like a fight or a perceived snub) and can change multiple times in a single day. While bipolar disorder is treated primarily with medication to balance chemicals, BPD is treated primarily with therapy to rewire emotional responses.
Borderline Personality Disorder Test — Why Causes Matter in Diagnosis
When you take a borderline personality disorder test, whether online or in a clinical setting, the questions are designed to uncover the developmental roots discussed above. Understanding what causes borderline personality disorder test results to lean high is key to the diagnostic process.
A professional assessment doesn’t just look at whether you meet the 9 traits of borderline personality disorder; it asks why those traits developed. For example:
- Childhood Questions: Screens often ask about your relationship with caregivers to identify early attachment disruptions.
- Trauma Screens: Questions about past abuse help clinicians determine if BPD is the primary diagnosis or if it co-occurs with PTSD.
- Emotional Patterns: Questions about how long a mood lasts (hours vs. weeks) help distinguish BPD from Bipolar Disorder.
Remember, a screening tool is the “smoke alarm,” but a professional evaluation is the “fire investigation” that confirms the cause.
Is Borderline Personality Disorder Dangerous?

The label of BPD often carries an unfair stigma of violence. However, when asking if borderline personality disorder dis angerous, the statistical reality is that the primary danger is to the individual themselves.
- Internalized Risk: The vast majority of “dangerous” behaviors associated with BPD are self-harm and suicidality. Up to 10% of individuals with BPD may die by suicide, making early intervention lifesaving.
- Impulsivity: Dangerous behaviors like reckless driving or substance abuse are often desperate attempts to “regulate” an unbearable emotional state, rather than a desire to harm others.
- Perception vs. Reality: While “borderline rage” can be frightening for loved ones, it is rarely premeditated or predatory. It is usually a “fight-or-flight” response to a perceived abandonment.
How to Treat Borderline Personality Disorder
For a long time, BPD was considered “untreatable.” Today, we know that is false. Modern borderline personality disorder treatments are highly effective at rewiring the brain’s emotional responses.
Dialectical Behavior Therapy (DBT)
The gold standard. DBT teaches four core skill sets: Mindfulness, Distress Tolerance, Emotion Regulation, and Interpersonal Effectiveness. It directly addresses the biological vulnerability of the disorder.
Mentalization-Based Therapy (MBT)
This therapy focuses on the psychological development cause. It helps patients “think about thinking,” allowing them to better understand their own emotions and the intentions of others before reacting impulsively.
New and Emerging Treatments
In 2026, research into Internal Family Systems (IFS) and neurofeedback is showing promise for BPD. These methods help individuals “unblend” from their most intense emotional parts and stabilize the overactive amygdala.
Is Borderline Personality Disorder Curable?
The question of whether borderline personality disorder is curable is often debated. While “cure” implies it disappears forever, clinicians prefer the term remission.
Recent longitudinal studies show that BPD has a better prognosis than many other mental health conditions. After 10 years of consistent treatment, up to 85% of patients no longer meet the diagnostic criteria for BPD. While the “emotional sensitivity” might always be a part of their temperament, the destructive behaviors and debilitating instability can go into full remission.
Can a Person With BPD Ever Be Happy?
Absolutely. Can a borderline ever be happy? Yes, and many find that their recovery leads to a life of “quiet joy” rather than constant chaos.
Recovery doesn’t mean you stop feeling deeply. It means you learn to ride the waves of emotion rather than being drowned by them. Many people with BPD in recovery use their natural high empathy and passion to excel in creative fields, social work, and parenting, finding a depth of meaning that others might never experience.
Why Understanding the Causes of BPD Reduces Stigma
When we understand what causes borderline personality disorder, we stop seeing it as a character flaw and start seeing it as a struggle for survival. No one chooses to be born with a sensitive nervous system, and no one chooses to be raised in an environment that can’t support them.
By focusing on the root causes, we replace judgment with empathy. This education-driven approach is the key to ensuring that people with BPD feel safe enough to seek the treatment they deserve.
Frequently Asked Questions
To conclude our deep dive into what causes borderline personality disorder, we have compiled the most common questions regarding the “why” behind the diagnosis. These answers integrate the latest 2026 clinical perspectives on the disorder.
What are the root causes of borderline personality disorder?
The root causes are essentially a “biosocial” interaction. This involves a biological foundation (genetic emotional sensitivity and a hyper-reactive amygdala) combined with an environmental trigger (an invalidating or traumatic childhood). The “root” is not just one thing, but the failure of the environment to teach a sensitive child how to manage their intense emotional world.
Can a single event cause BPD?
Generally, no. While a single, massive trauma can lead to PTSD, BPD is a personality-based disorder that develops over the years. It is usually the result of chronic, repetitive experiences—such as ongoing emotional neglect or a long-term invalidating household—that shape how a person views themselves and others over the course of their development.
Is BPD caused by bad parenting?
This is a harmful myth. While an “invalidating environment” is a factor, this does not always mean “bad” or “abusive” parenting. Sometimes, it is simply a “mismatch” between a very sensitive child and parents who are more stoic or less emotionally expressive. The parents may be loving and well-intentioned, but simply lack the specific tools needed to coach a child with such high emotional intensity.
Why do some people with trauma get PTSD and others get BPD?
This comes down to the biological “nature” part of the equation. Someone born with a naturally resilient temperament may develop PTSD symptoms (like flashbacks or hypervigilance) after trauma. However, someone born with an emotionally sensitive temperament is more likely to develop the identity confusion and relationship instability characteristic of BPD following similar trauma.
Can BPD develop in adulthood?
While the symptoms may only become unmanageable or “explosive” in adulthood—often triggered by the stress of college, moving away, or a major breakup—the seeds of the disorder are almost always sown during childhood and adolescence. BPD is a developmental condition, meaning the foundations are laid during the years when personality is most plastic.
Conclusion
Understanding what causes borderline personality disorder is the ultimate tool for de-stigmatization. For too long, the “borderline” label has been used to describe people who were seen as “manipulative” or “attention-seeking.” By looking at the neurobiology of the amygdala, the statistics of childhood trauma, and the impact of invalidating environments, we see a much more accurate picture.
Individuals with BPD are not “behaving badly”; they are individuals whose internal “smoke alarm” is permanently stuck on high. Their behaviors—while often self-destructive—are usually desperate attempts to regulate a level of emotional pain that most people will never have to experience.
Authoritative References
1. National Institute of Mental Health (NIMH) – Borderline Personality Disorder
2. Harvard Medical School (Harvard Health) – Borderline Personality Disorder
3. National Library of Medicine (NCBI) – The Neurobiology of BPD
4. National Education Alliance for Borderline Personality Disorder (NEA-BPD)
5. The Lancet –Borderline Personality Disorder (Clinical Seminar)
Subscribe to Our Newsletter
Get mental health tips, updates, and resources delivered to your inbox.