Do i need therapy for bipolar disorder? Therapy, Medication, and Living a Normal Life

Receiving a diagnosis of bipolar disorder can feel like standing at the base of an insurmountable mountain. The shifting tides of mood—from the electrifying highs of mania to the paralyzing depths of depression—can make the concept of “stability” seem like a distant dream. However, the modern clinical landscape has transformed what it means to live with this condition. Today, treatment options for bipolar disorder are more sophisticated, personalized, and effective than ever before.
Bipolar disorder is not a character flaw or a temporary emotional reaction; it is a chronic neurological condition that requires a multi-layered, lifelong management strategy. The most effective treatment for bipolar disorder is rarely found in a single pill or a solitary therapy session. Instead, it is built upon three essential pillars: pharmacological intervention to stabilize brain chemistry, psychotherapy to develop coping mechanisms, and a rigorous daily routine to anchor the body’s internal rhythms.
This guide provides an exhaustive look at the journey from diagnosis to long-term stability. Whether you are navigating your first episode or seeking to refine a long-standing treatment plan, understanding the medical guidelines and lifestyle adjustments available today is the first step toward reclaiming your life. With the right tools, “living a normal life” is not just a possibility—it is the expected outcome for the majority of patients.
What Is Bipolar Disorder and What Causes It?
At its core, bipolar disorder is a mood disorder characterized by extreme shifts in energy, activity levels, and the ability to carry out day-to-day tasks. But to treat it effectively, we must look beneath the surface at what causes bipolar disorder. It is fundamentally a biological “glitch” in the brain’s regulatory systems.
Current research points to three primary drivers:
- Brain Chemistry and Circuitry: Individuals with bipolar disorder often have physical changes in their brains. Specifically, there are imbalances in neurotransmitters—the brain’s chemical messengers—such as dopamine, serotonin, and norepinephrine. Furthermore, the circuits that regulate emotion and reward processing may be “hyper-sensitive” or “under-responsive” depending on the phase of the illness.
- Genetics: Bipolar disorder tends to run in families. If a first-degree relative (parent or sibling) has the condition, the likelihood of developing it increases significantly. However, genetics is not destiny; most people with a family history do not develop the disorder, suggesting that environmental factors play a key role.
- Environmental Triggers: High-stress events, such as the loss of a loved one, a traumatic experience, or even a major positive life change like a promotion, can act as a catalyst for the first episode. Sleep deprivation is perhaps the most potent environmental trigger, capable of “flipping the switch” from a stable mood into a manic state.
Understanding these causes helps remove the stigma of the diagnosis. It is a medical condition of the brain’s “thermostat,” and like any other chronic illness, it requires medical management rather than just “willpower.”
Bipolar Disorder Symptoms (Including in Females)
Symptoms of bipolar disorder vary significantly between individuals and can manifest differently based on gender, age, and subtype. While the hallmark of the condition is the “mood swing,” the symptoms are often more complex than just being happy or sad.
Bipolar Disorder Symptoms in Females
Recent studies have highlighted that women often experience a unique clinical profile. Bipolar disorder symptoms in females are more likely to involve:
- Depressive Dominance: Women tend to spend more time in the depressive phase than men.
- Rapid Cycling: Defined as having four or more mood episodes within a year, rapid cycling is more prevalent in females.
- Hormonal Influence: Menstrual cycles, pregnancy, and menopause can significantly impact mood stability. Postpartum psychosis is also a higher risk for women with a history of bipolar disorder.
- Comorbid Conditions: Women with bipolar disorder have higher rates of thyroid disease, migraine, and anxiety disorders compared to men.
Common Symptoms Across Genders
Regardless of gender, the symptoms are divided into two distinct “poles”:
The Manic/Hypomanic Phase:
- Abnormally high energy or agitation.
- Exaggerated sense of well-being and self-confidence (grandiosity).
- Decreased need for sleep (feeling rested after only 3 hours).
- Racing thoughts and talking unusually fast (pressured speech).
- Poor decision-making—spending sprees, sexual risks, or foolish investments.
The Depressive Phase:
- Overwhelming sadness, hopelessness, or emptiness.
- Loss of interest in almost all activities (anhedonia).
- Significant weight loss or gain.
- Either insomnia or sleeping too much (hypersomnia).
- Fatigue or loss of energy that feels physical (leaden paralysis).
- Feelings of worthlessness or excessive guilt.
Bipolar 1 vs Bipolar 2 — Key Differences That Affect Treatment
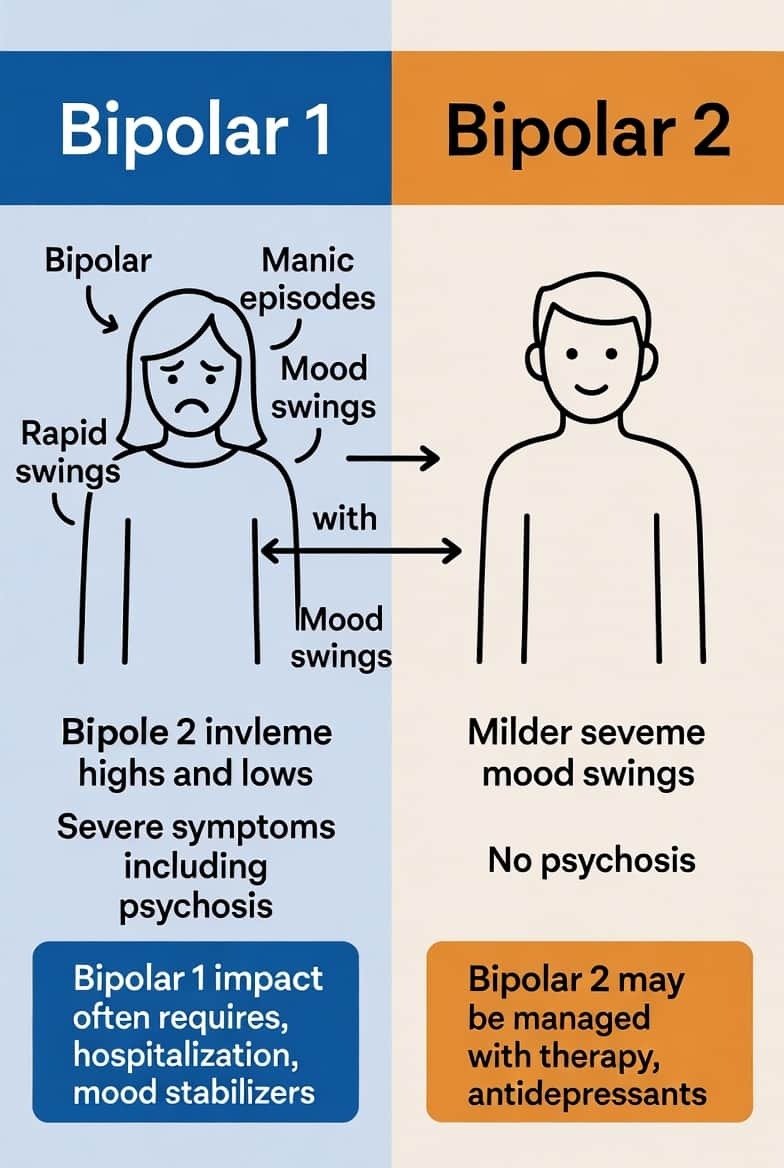
Understanding the bipolar 2 and 1 difference is critical because it dictates the primary focus of the treatment plan. While both involve extreme mood shifts, the intensity and duration of the “highs” vary.
Bipolar 1 Disorder: This is defined by the occurrence of at least one manic episode. Manic episodes in Bipolar 1 can be severe and dangerous, often requiring hospitalization. While depressive episodes are common, they are not technically required for a Bipolar 1 diagnosis. Treatment here often focuses heavily on “capping” the mania to prevent life-altering impulsive decisions.
Bipolar 2 Disorder: Individuals with Bipolar 2 experience “hypomania”—a less severe version of mania that doesn’t usually cause significant impairment in social or work functioning. However, Bipolar 2 is characterized by much longer and more frequent periods of severe depression. In this subtype, the treatment focus is often on lifting the chronic “lows” without triggering a hypomanic “overshoot.”
Misdiagnosis is common in Bipolar 2 because patients often enjoy the productivity of hypomania and only seek help during the depressive phase. This leads many to be misdiagnosed with standard Major Depressive Disorder (MDD), which can lead to improper treatment.
How Is Bipolar Disorder Diagnosed?
There is no blood test or brain scan that can definitively say, “You have bipolar disorder.” Instead, the process of diagnosing bipolar disorder is clinical and relies on a detailed history of symptoms.
The diagnostic process typically involves:
- Physical Exam: To rule out other conditions, like thyroid problems that might mimic mood swings.
- Psychiatric Assessment: A doctor or mental health professional will talk to you about your thoughts, feelings, and behavior patterns. You may be asked to fill out a mood chart or a psychological self-assessment.
- DSM-5 Criteria: Clinicians compare your symptoms to the criteria listed in the Diagnostic and Statistical Manual of Mental Disorders (DSM-5), published by the American Psychiatric Association.
- Mood Charting: Because memories can be unreliable during a mood episode, a doctor may ask you to keep a daily record of your mood, sleep patterns, and energy levels over several weeks to look for the “cycling” characteristic of the disorder.
Because bipolar disorder can look like ADHD, borderline personality disorder, or clinical depression, the diagnostic journey can sometimes take years. Patience and honesty with your care team are vital during this phase.
Do Bipolar People Need Therapy?
A frequent question among newly diagnosed patients is: Do bipolar people need therapy if they are already taking medication? The answer is a resounding yes. While medication stabilizes the biological foundation, it does not teach you how to navigate a world that is often stressful and unpredictable.
Do I Need Therapy for Bipolar Disorder?
Yes. Medication can stop the “fire” of mania or the “ice” of depression, but therapy provides the “architecture” for a stable life. Therapy helps you:
- Recognize early “prodromal” symptoms (warning signs) before a full episode begins.
- Manage the trauma and regret that often follow a manic episode.
- Improve relationships that may have been strained by mood volatility.
- Develop “social rhythm” strategies to maintain a healthy routine.
What Therapy Helps Most?
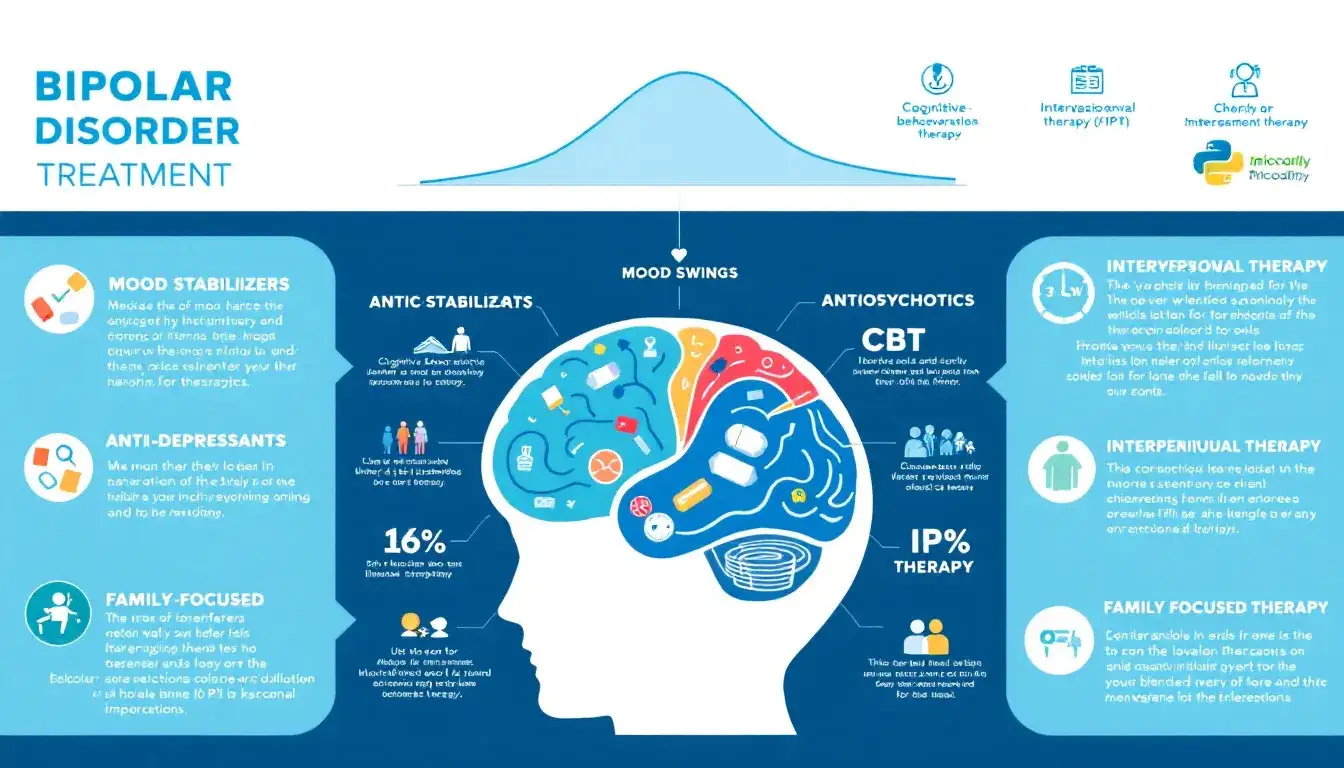
Several evidence-based therapies are specifically designed for bipolar disorder:
- Cognitive Behavioral Therapy (CBT): Focuses on identifying and changing negative thought patterns and behaviors. It is highly effective for managing the depressive phase.
- Dialectical Behavior Therapy (DBT): Excellent for emotional regulation and managing the intense irritability or suicidal ideation that can occur during mixed states.
- Interpersonal and Social Rhythm Therapy (IPSRT): This is perhaps the most important therapy for bipolar patients. It focuses on stabilizing daily rhythms—eating, sleeping, and exercising—to keep the brain’s internal clock in sync.
Psychotherapy and Structured Treatment Plans

While talk therapy is often viewed as a general supportive tool, for bipolar disorder, it must be highly structured. A formal treatment plan for bipolar disorder pdf or digital document, often serves as the “operating manual” for the patient’s life. These plans move beyond abstract feelings and focus on data-driven management.
A structured plan typically includes:
- Relapse Prevention Mapping: Identifying your specific “red flags” (e.g., spending more money, sleeping less, or sudden irritability).
- Crisis Protocols: A clear set of instructions for what to do—and who to call—if you or a loved one notices symptoms reaching a dangerous level.
- Routine Checklists: Daily non-negotiables that keep the brain’s “social rhythm” stable.
Clinicians often provide a psychotherapy for bipolar disorder pdf that includes mood-tracking charts. These allow patients to visualize the correlation between their sleep patterns and their mood shifts. By documenting these variables, you and your therapist can identify triggers—such as high-stress work projects or seasonal light changes—and adjust your strategies before an episode fully takes hold.
Medication Options for Bipolar Disorder
For the vast majority of people, medication is the bedrock of treatment. Because bipolar disorder is a biological “energy crisis,” talk therapy alone is rarely enough to prevent the cycling of the brain’s chemistry. Understanding your treatment options for bipolar disorder requires a look at three main classes of drugs.
Mood Stabilizers and Antipsychotics
- Lithium: The oldest and still one of the most effective treatments, Lithium is a natural salt that has a unique ability to reduce suicidal ideation and “cap” mania. It requires regular blood tests to ensure levels stay within a therapeutic range.
- Anticonvulsants (Mood Stabilizers): Drugs like Valproate, Lamotrigine, and Carbamazepine are frequently used. Lamotrigine is particularly noted for its effectiveness in preventing bipolar depression without causing a “switch” into mania.
- Atypical Antipsychotics: Modern medications such as Quetiapine, Risperidone, and Aripiprazole are often used to treat acute mania. Many of these have been refined to also treat bipolar depression effectively.
Strong Bipolar Medication — What That Really Means
When patients ask for strong bipolar medication, they are often referring to “rescue medications” used during a severe crisis. These are typically high-potency antipsychotics or benzodiazepines used to stop a manic episode that involves psychosis or severe sleep deprivation. While these are “strong” in terms of immediate effect, the “strongest” treatment for long-term health is actually the consistent, low-dose maintenance of mood stabilizers that prevent the crisis from happening in the first place.
Best Antidepressants for Bipolar — What to Know

The search for the best antidepressants for bipolar disorder is one of the most common, yet most controversial, topics in psychiatry. In standard depression, antidepressants are the primary tool. In bipolar disorder, they can be like pouring gasoline on a fire.
The Risk of Mania
The primary danger of using antidepressants (like SSRIs or SNRIs) in bipolar patients is the risk of “switching.” This occurs when the antidepressant pushes the mood too far upward, triggering a manic or hypomanic episode. Furthermore, antidepressants can sometimes cause “rapid cycling,” where the patient begins to flip between moods every few weeks or even days.
Safe Usage Guidelines
Current bipolar disorder treatment guidelines suggest that antidepressants should:
- Never be used alone: They must be paired with a mood stabilizer or an antipsychotic to act as a “buffer.”
- Be used for short durations: Once the depressive episode lifts, many doctors taper the antidepressant to avoid destabilizing the patient.
- Be closely monitored: If you notice sudden energy, racing thoughts, or decreased need for sleep while taking an antidepressant, it is a medical emergency that requires an immediate call to your psychiatrist.
Bipolar Disorder Treatment Guidelines Explained Simply
Navigating mental health care can feel like guesswork, but it is actually guided by rigorous clinical standards. The bipolar disorder treatment guidelines (established by organizations like the APA and NICE) follow a logical “step-care” model.
- Acute Phase: The immediate goal is to stop a crisis. If you are manic, the goal is sedation and safety. If you are severely depressed, the goal is to prevent self-harm and restore basic function.
- Stabilization Phase: Once the crisis has passed, the focus shifts to finding the right medication dosage that minimizes side effects while keeping moods within a “normal” range.
- Maintenance Phase: This is the long-term phase where the goal is relapse prevention. This is where therapy and routine become just as important as the medication.
These guidelines emphasize that treatment is a partnership. A good psychiatrist won’t just tell you what to take; they will work with you to find a balance that allows you to feel like yourself, not a “zombie” or a “muted” version of your personality.
Treatment Goals for Bipolar Disorder
What does “success” look like? Defining the treatment goals for bipolar disorder is essential for staying motivated.
- Symptom Remission: The primary goal is to reach a state of “euthymia”—a stable, normal mood where you are neither high nor low.
- Functional Recovery: This means being able to return to work, finish school, or maintain your roles as a parent or partner.
- Reducing Episode Frequency: Over time, the goal is to make the “gap” between episodes longer and the episodes themselves shorter and less severe.
- Minimizing Side Effects: A major goal is finding a treatment plan that doesn’t interfere with your physical health, weight, or cognitive clarity.
By having clear goals, you can have more productive conversations with your care team. If your mood is stable but you are too tired to work, your treatment goal hasn’t been fully met, and adjustments are needed.
Do Bipolar People Need Routine?

If medication is the foundation and therapy is the structure, routine is the “anchor.” So, do bipolar people need routine? The clinical answer is a definitive yes. The bipolar brain has a “leaky” internal clock; it struggles to regulate its own energy levels without external cues.
The Power of Social Rhythms
Consistency in daily habits acts as an “external pacemaker.” When you eat at the same time, work at the same time, and socialize at the same time, you are sending signals to your brain that it is safe to maintain a steady level of neurotransmitters.
- Sleep-Wake Consistency: This is the most vital routine. Even a two-hour difference in your wake-up time on weekends can be enough to trigger a mood shift.
- Meal Timing: Regular meals prevent blood sugar spikes and crashes, which can mimic or trigger irritability and fatigue.
- Activity Levels: Moderate, regular exercise is better than intense, sporadic bursts, which can sometimes trigger hypomania.
How to Naturally Deal With Bipolar Disorder (Alongside Treatment)
While medication is the “engine” of recovery, lifestyle modifications are the “fuel.” In 2026, the medical community increasingly recognizes that “natural” interventions are not replacements for medicine, but essential enhancers.
- Nutritional Psychiatry: Emerging research suggests that the bipolar brain is highly sensitive to inflammation. A diet rich in Omega-3 fatty acids (found in fish and flaxseed) can act as a natural neuro-protector, potentially reducing the intensity of depressive dips.
- Targeted Supplementation: Under medical supervision, supplements like Magnesium and Vitamin D are often used to support the nervous system. However, patients must exercise extreme caution with herbs like St. John’s Wort, which can trigger manic “switch” reactions.
- Mindfulness and Interception: Developing “interceptive awareness”—the ability to feel subtle shifts in your body’s energy—allows you to catch a mood shift days before it becomes an episode. Practices like Yoga or Tai Chi help bridge the gap between physical sensation and emotional state.
How a Person With Bipolar Thinks
Understanding how a person with bipolar disorder thinks is the key to both self-management and interpersonal empathy. Mood episodes don’t just change how you feel; they rewire how you process logic.
Thinking During Mania
- Grandiosity: The “internal volume” of self-confidence is turned up to a maximum. Ideas feel world-changing, and the consequences of actions (like spending or risky behavior) feel non-existent.
- Racing Thoughts: The brain moves faster than the tongue. Connections between unrelated ideas seem obvious and brilliant, leading to “flight of ideas.”
Thinking During Depression
- Cognitive Distortions: The brain falls into “all-or-nothing” thinking. A small mistake at work is interpreted as proof of total worthlessness (catastrophizing).
- Emotional Reasoning: “I feel like a burden, therefore I am a burden.” This logical fallacy is the primary driver of social withdrawal.
Is Bipolar Disorder Dangerous?
When people ask, is bipolar disorder dangerous?, the answer is nuanced. The danger lies not in the person, but in the untreated episodes.
- Self-Harm and Suicide Risk: Bipolar disorder has one of the highest rates of self-harm among mental health conditions, often occurring during “mixed states” where one feels the despair of depression but the high energy of mania.
- Physical Health Risks: Long-term instability can lead to secondary issues like cardiovascular disease or metabolic syndrome, often due to the high stress of mood cycles.
- Mitigation: The “danger” is drastically reduced—near baseline levels—when a person is adherent to a bipolar disorder treatment plan. Medication and therapy are the primary safety nets that prevent these risks from manifesting.
Can Manic Depression Be Cured?

A common source of grief for the newly diagnosed is the realization that manic depression cannot be cured in the traditional sense. It is a lifelong, chronic condition of the brain’s regulatory system.
However, “remission” is a very real and attainable goal. In the same way that a person manages diabetes with insulin and diet, a person with bipolar disorder manages their chemistry with medication and routine. With 2026’s advancements in precision psychiatry, many patients go years, even decades, without a major symptomatic breakthrough.
Can You Live a Normal Life With Bipolar Disorder?
The ultimate question for many is: How can I live a normal life with bipolar disorder? The answer is that “normal” is a subjective target. Millions of people with bipolar disorder are successful parents, CEOs, doctors, and artists.
Living a “normal” life with bipolar disorder simply means your life is no longer defined by the disorder. You may need to prioritize sleep more than your peers, and you may need to avoid alcohol or late-night shifts, but these are small adjustments in exchange for a full, vibrant life. Stability is not the absence of disorder; it is the mastery over it.
Building a Sustainable Bipolar Treatment Plan
Building a life beyond bipolar disorder is a project of persistence.
- Treatment is a Partnership: Work with your psychiatrist to find a medication balance that doesn’t just “numb” you but allows you to function.
- Routine is Medicine: Treat your sleep schedule as strictly as your medication schedule.
- Therapy is the Manual: Use your sessions to build a “toolbox” for when the clouds inevitably gather.
Stability is possible. Recovery is expected. Your diagnosis is the beginning of a more intentional, managed, and ultimately successful life.
Frequently Asked Questions
Can I stop taking my medication once I feel stable?
No. This is the most common reason for relapse. Feeling “normal” is a sign that the medication is working, not that the disorder has disappeared. Stopping medication suddenly can trigger a severe manic episode or a “crash” into deep depression.
What is the “best” treatment for bipolar disorder?
While everyone is different, the gold standard is Lithium or a combination of an atypical antipsychotic and a mood stabilizer, paired with Interpersonal and Social Rhythm Therapy (IPSRT).
Do bipolar people need therapy even if they don’t feel depressed?
Yes. Therapy during stable periods (euthymia) focuses on “relapse prevention.” It helps you refine your routine and identify “prodromes”—tiny, early warning signs of a mood shift that you might miss on your own.
Are there natural ways to treat bipolar disorder?
Natural strategies like Omega-3 supplementation, strict sleep hygiene, and stress reduction are excellent supportive tools. However, they cannot replace medication because they do not have the same “mood-capping” power needed to manage the biological shifts of the disorder.
How do I know if I have Bipolar 1 or Bipolar 2?
A psychiatrist makes this distinction based on the intensity of your “highs.” If you have ever had a manic episode that lasted at least a week or required hospitalization, it is Bipolar 1. If your “highs” are productive but don’t cause major life destruction (hypomania), it is Bipolar 2.
Why are antidepressants considered dangerous for bipolar disorder?
In standard depression, the brain is “low.” In bipolar disorder, the brain is “unstable.” Antidepressants can push the mood too far up, causing a “switch” into mania or leading to “rapid cycling,” where your moods flip-flop uncontrollably.
Is bipolar disorder a life sentence?
It is a lifelong condition, but it is not a sentence to a diminished life. With modern precision medicine and a structured lifestyle, the prognosis is excellent. Most people with bipolar disorder live full, productive, and “normal” lives.
Conclusion
Building a sustainable bipolar disorder treatment plan is perhaps the most significant project you will ever undertake. It is a transition from being a passenger to being the pilot of your own neurochemistry. While the diagnosis may be lifelong, the acute suffering associated with it does not have to be.
By integrating the clinical standards of the most effective treatment for bipolar disorder—combining targeted medication with the structural support of psychotherapy—you create a foundation that can withstand the inevitable stresses of life. When you add the “pacemaker” of a strict daily routine and the “fuel” of healthy lifestyle choices, you move from the instability of the past into a future of consistent, predictable wellness.
Stability is not a destination where the disorder disappears; it is a state of mastery where you have the tools to manage the shifts before they manage you. Thousands of people are currently living a normal life with bipolar disorder, thriving in their careers and finding deep fulfillment in their relationships. With persistence, a specialized care team, and the strategies outlined in this guide, you can be one of them.
Authoritative References
- National Institute of Mental Health (NIMH):Comprehensive Guide to Bipolar Disorder
- Mayo Clinic:Diagnosis and Treatment Protocols for Bipolar I and II
- American Psychiatric Association (APA):Practice Guidelines for the Treatment of Patients with Bipolar Disorder
- Mayo Clinic:Bipolar Disorder Diagnosis & Treatment
- DBSA: Peer-Led Support Groups and Wellness Recovery Action Plans (WRAP)
Subscribe to Our Newsletter
Get mental health tips, updates, and resources delivered to your inbox.