Major Depressive Disorder Medications: Treatments, Options, and Side Effects
Major Depressive Disorder (MDD) is more than just a period of sadness or a “rough patch.” It is a profound clinical condition that affects nearly every aspect of an individual’s life, from their physical health to their social connections and professional productivity. As mental health awareness grows, the focus has shifted toward evidence-based solutions that offer tangible relief.
Central to this effort is the use of pharmacotherapy. This guide provides an exhaustive look at major depressive disorder medication, exploring how these treatments work, the options available, and what patients and clinicians should consider when building a recovery plan.
Understanding Major Depressive Disorder
What is major depressive disorder? At its core, MDD is a mood disorder characterized by at least two weeks of pervasive low mood, low self-esteem, and a loss of interest or pleasure in normally enjoyable activities. It is often accompanied by physical symptoms such as changes in appetite, sleep disturbances, and a persistent lack of energy.
Unlike standard grief or sadness, MDD is persistent and often lacks an immediate external “cause,” making it a complex biological and psychological challenge.
When patients ask how to treat major depressive disorder, the answer is rarely singular. The gold standard of care involves a “biopsychosocial” approach. This means addressing the biological roots through medication, the psychological aspects through therapy, and the social factors through lifestyle changes and support systems.
While therapy provides the tools to manage thoughts and behaviors, medication often provides the neurological “floor” necessary for those tools to be effective.
Why Medication is a Cornerstone of Treatment
The shift in modern psychiatry has been heavily influenced by the “chemical imbalance” theory, though our understanding has evolved into a more nuanced view of neuroplasticity and brain circuitry.
Dr. Zoey believes that major depressive disorder is caused by neurotransmitter abnormalities and is most effectively treated with medication, a sentiment shared by many in the clinical community who observe the transformative power of antidepressants.
The Biochemical Basis of MDD
Research suggests that MDD is closely linked to the dysregulation of neurotransmitters—the brain’s chemical messengers. The primary culprits are usually:
- Serotonin: Regulates mood, sleep, and appetite.
- Norepinephrine: Influences energy levels and alertness.
- Dopamine: Drives the brain’s reward and pleasure centers.
Restoring Function Through Pharmacotherapy
Evidence-based treatment for depression focuses on restoring the balance of these chemicals. Antidepressants do not simply “make you happy”; rather, they modulate the availability of these neurotransmitters to improve the brain’s ability to regulate emotion.
For many, medication acts as a bridge, reducing the severity of symptoms so that the best therapeutic interventions for depression, such as Cognitive Behavioral Therapy (CBT), can take hold. Without pharmacotherapy, patients with severe depression may find it impossible to engage in the very activities—like exercise or social interaction—that promote recovery.
Overview of Major Depressive Disorder Medications
The landscape of major depressive disorder medication options is vast, categorized by how they interact with the brain. Choosing the right antidepressants for major depressive disorder requires understanding these specific classes and their mechanisms of action.
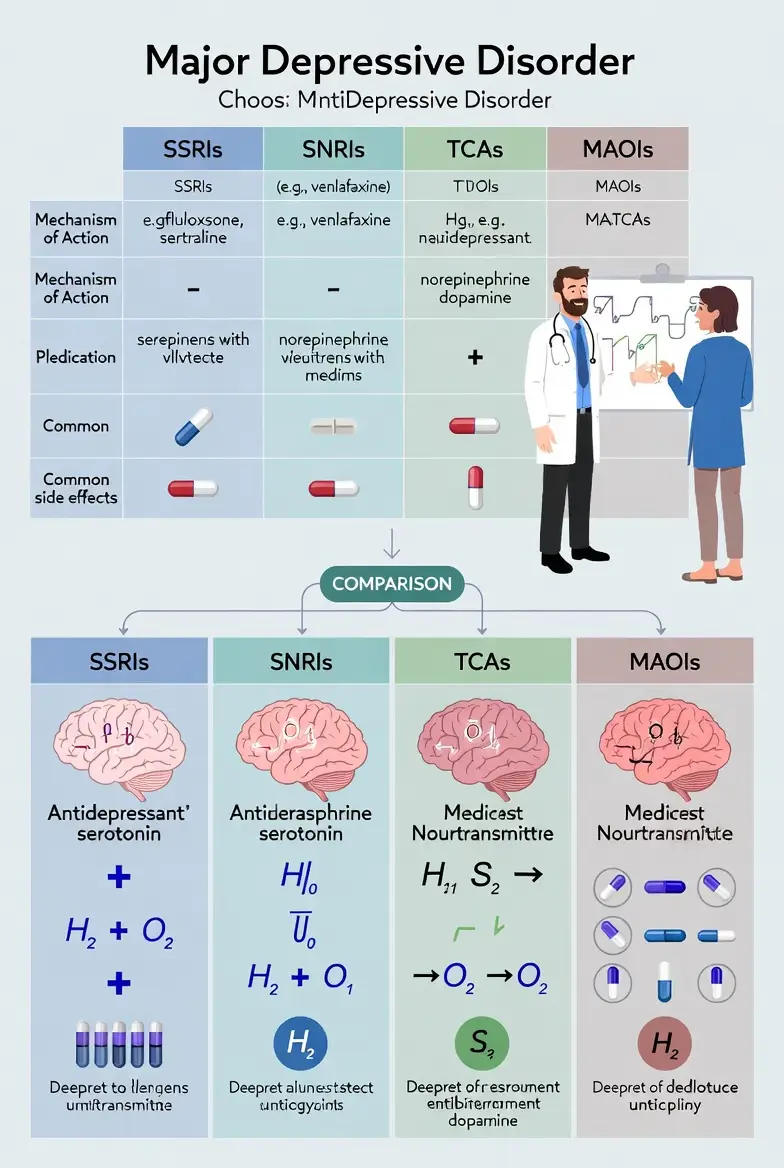
SSRIs (Selective Serotonin Reuptake Inhibitors)
SSRIs are typically the first-line FDA-approved major depressive disorder medication. They work by blocking the reabsorption (reuptake) of serotonin in the brain, making more serotonin available to improve message transmission between neurons. They are favored for having fewer side effects than older drug classes.
SNRIs (Serotonin-Norepinephrine Reuptake Inhibitors)
SNRIs block the reuptake of both serotonin and norepinephrine. These are often prescribed when SSRIs are insufficient, particularly for patients who also experience chronic pain or significant lethargy.
Atypical Antidepressants
These medications do not fit neatly into other categories. For example, some may target dopamine or specific serotonin receptors differently. They are frequently used as “add-on” treatments or for patients who experience sexual side effects from SSRIs.
Older Generations: Tricyclics and MAOIs
Tricyclic antidepressants (TCAs) and Monoamine Oxidase Inhibitors (MAOIs) were the primary treatments decades ago. While highly effective, they are now reserved for “treatment-resistant depression” because they require strict dietary restrictions (in the case of MAOIs) and carry a higher risk of severe side effects and toxicity in overdose.
Full List of MDD Medications: Generic and Brand Names
Navigating a major depressive disorder medication list can be overwhelming due to the overlap of major depressive disorder medication names and their corresponding major depressive disorder medication brands. Below is a comprehensive list of major depressive disorder medications categorized by drug class.
i. Popular First-Line SSRIs
- Sertraline (Zoloft): Frequently, the most prescribed major depressive disorder medication Zolof,t is known for its versatility and safety profile.
- Escitalopram (Lexapro): The major depressive disorder medication Lexapro is often praised for being “cleaner,” meaning it has fewer drug-to-drug interactions.
- Fluoxetine (Prozac): The first famous SSRI, often used because of its long “half-life,” making it easier to taper off.
- Paroxetine (Paxil): Often used for depression accompanied by high levels of anxiety.
- Citalopram (Celexa): A reliable, cost-effective option similar to Lexapro.
ii. Common SNRIs and Atypicals
- Duloxetine (Cymbalta): Excellent for depression paired with physical pain or fibromyalgia.
- Venlafaxine (Effexor): Effective for severe depression but requires careful monitoring of blood pressure.
- Bupropion (Wellbutrin): Unique because it targets norepinephrine and dopamine; it is often used to avoid the weight gain and sexual dysfunction associated with other drugs.
- Mirtazapine (Remeron): Frequently used for patients who struggle with insomnia and weight loss due to depression.
iii. New and Emerging Medications
The search for a new major depressive disorder medication has led to breakthroughs beyond traditional daily pills:
- Vortioxetine (Trintellix): A multimodal antidepressant that may improve cognitive symptoms like “brain fog.”
- Esketamine (Spravato): An FDA-approved nasal spray for treatment-resistant depression that works on the glutamate system, providing rapid relief where others have failed.
- Auvelity: A recently approved fast-acting oral medication combining bupropion and dextromethorphan.
Choosing the Best Medication
Determining the best major depressive disorder medication is not a “one-size-fits-all” process. What serves as the strongest antidepressant for severe depression for one person might be ineffective for another. Clinicians use a personalized approach to answer the question: What is the best medication for major depressive disorder?
As we move further into 2026, the landscape of selection has shifted from “trial and error” toward a more data-driven, patient-centered model. Because most standard antidepressants have roughly equal efficacy in broad clinical trials, the choice often hinges on matching the drug’s specific “fingerprint” to the patient’s unique biological and lifestyle needs.
Factors Influencing the Decision
a. Symptom Cluster Matching: Depression presents differently in every individual. If a patient is agitated, anxious, and struggling with insomnia, a sedating antidepressant like Mirtazapine is often the first choice. Conversely, if a patient suffers from “melancholic” or “atypical” depression characterized by extreme lethargy and oversleeping, an “activating” medication like Bupropion is preferred to help restore energy and motivation.
b. Side Effect Tolerance: This is often the primary driver of shared decision-making. A patient who is concerned about sexual health may steer clear of SSRIs in favor of Bupropion or Vortioxetine. Someone prioritizing the avoidance of weight gain will typically avoid Paroxetine or Mirtazapine.
By selecting a medication with a side-effect profile the patient can live with, clinicians significantly improve long-term adherence.
c. Comorbidities: Many patients live with “dual diagnoses” or physical health issues. For example:
- Chronic Pain/Neuropathy: An SNRI like Duloxetine (Cymbalta) is often chosen because it treats both the mood disorder and the physical pain signals.
- Anxiety Disorders: While many SSRIs treat both, some (like Sertraline) are particularly effective for comorbid Panic Disorder or OCD.
- Smoking Cessation: Bupropion is frequently used for patients who wish to quit smoking while treating their depression.
- Family History and Genetics: If a biological relative responded exceptionally well to a specific medication, there is a higher statistical likelihood that the patient will too. Furthermore, Pharmacogenomic (PGx) testing has become a mainstream tool in 2026. These tests analyze the patient’s CYP450 enzymes to predict how quickly they metabolize certain drugs, helping to avoid medications that might build up to toxic levels or be processed too quickly to work.
The 2026 Selection Standard: Shared Decision-Making
The modern approach rejects the “doctor-orders-patient-follows” dynamic. Instead, clinicians provide a menu of evidence-based treatment options for depression, explaining the pros and cons of each.
This collaboration ensures the patient feels a sense of agency, which research shows is a powerful predictor of successful recovery. If the first choice doesn’t result in remission within 4–8 weeks, the plan is immediately adjusted rather than waiting months for a result that isn’t coming.
Medication Use in Specific Populations
Because the biological profile of a patient changes across the lifespan, a major depressive disorder medication for kids will be approached differently than one for a 70-year-old. Safety, metabolic rate, and psychological development all play critical roles in prescribing.
Pediatric and Adolescent Considerations
Treating depression in young people requires extreme caution. Currently, Fluoxetine (Prozac) and Escitalopram (Lexapro) are the only two antidepressants with broad FDA approval for treating MDD in pediatric patients.
- The Black Box Warning: All antidepressants carry a mandated “black box” warning for children and young adults up to age 24. This warning highlights a statistically increased risk of suicidal thoughts and behaviors during the first few weeks of treatment.
- Monitoring: Close clinical supervision is mandatory, particularly during dose adjustments, to monitor for “activation” (agitation, restlessness, or increased impulsivity).
Geriatric Considerations
For the elderly, the clinical mantra is “start low and go slow.”
- Metabolism: Reduced kidney and liver function means that a major depressive disorder medication for adults in their 30s might reach toxic levels in a 75-year-old at the same dosage.
- Fall Risks: Older antidepressants (TCAs) and even some SNRIs are associated with orthostatic hypotension (a drop in blood pressure when standing), which significantly increases the risk of falls and fractures. Sertraline (Zoloft) and Lexapro are often preferred due to their safer cardiac profiles.
Pregnancy and Lactation
The decision to use medication during pregnancy involves weighing the risks of the drug against the risks of untreated maternal depression (which can lead to low birth weight and developmental issues). Most SSRIs are considered relatively safe, though Paroxetine (Paxil) is often avoided due to a slightly higher risk of fetal heart defects. During breastfeeding, medications with low “infant milk-to-plasma ratios” like Sertraline are typically the first choice.
Side Effects and Safety Profile
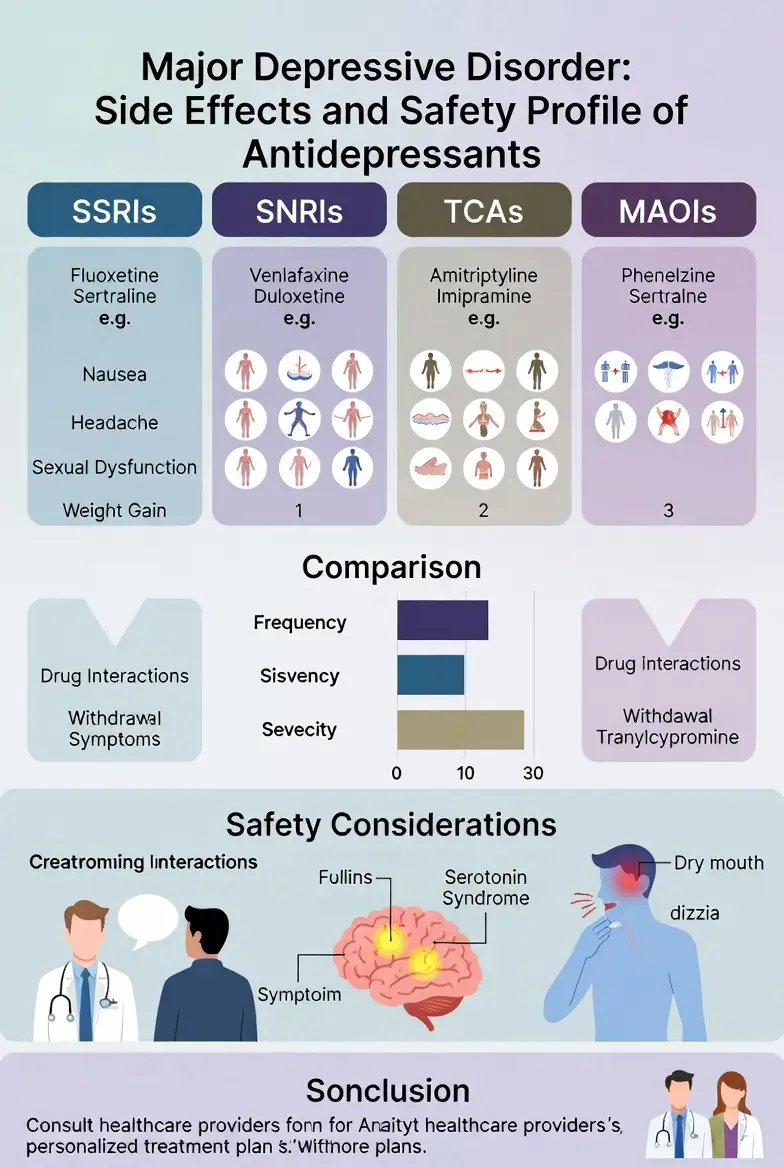
Understanding major depressive disorder medication side effects is essential for long-term adherence. Most patients experience mild side effects that dissipate within the first two weeks as the body adjusts, but some require active medication management.
Common vs. Serious Side Effects
| Side Effect Type | Common Examples | Management Strategy |
| Gastrointestinal | Nausea, diarrhea, dry mouth | Take with food; stay hydrated. |
| Neurological | Headache, dizziness, insomnia | Shift dosing to morning or night. |
| Sexual | Low libido, delayed orgasm | Discuss dose adjustment or “add-on” meds. |
| Metabolic | Increased appetite, weight gain | Monitor diet and physical activity. |
Serious Safety Concerns
- Serotonin Syndrome: A rare but potentially life-threatening condition caused by an excess of serotonin. Symptoms include high fever, muscle rigidity, and rapid heart rate. This often occurs when combining two serotonergic drugs (e.g., an SSRI and a migraine medication).
- Withdrawal (Discontinuation Syndrome): Abruptly stopping an antidepressant can lead to “brain zaps,” flu-like symptoms, and intense irritability. Always taper off under medical supervision.
Cost Considerations
The major depressive disorder medication can be a significant barrier to care. Fortunately, as of 2026, many of the most effective first-line treatments are available as affordable generics.
- Generic vs. Brand Name: Generic versions of Zoloft, Prozac, and Lexapro can often be filled for as little as $5–$20 for a 30-day supply. In contrast, newer brand-name medications like Trintellix or Auvelity can cost hundreds of dollars without insurance.
- Insurance and Medicare: Most commercial insurance plans prioritize generics. Under recent 2026 updates to the Inflation Reduction Act, Medicare has also expanded its ability to negotiate lower prices for certain high-cost psychiatric drugs.
- Patient Assistance Programs (PAPs): Pharmaceutical companies often offer programs to provide free or discounted medications to uninsured or low-income patients. Websites like NeedyMeds can help identify these opportunities.
Non-Medication Options
While this guide focuses on pharmacotherapy, how to treat major depressive disorder without medication (or in conjunction with it) is a vital part of the conversation. Interventions to help with depression extend beyond the pharmacy.
Psychotherapy: The Necessary Companion
Best therapeutic interventions for depression, like Cognitive Behavioral Therapy (CBT) and Interpersonal Therapy (IPT), address the thought patterns and relational issues that fuel MDD. Clinical data consistently show that the combination of medication and therapy is more effective than either treatment alone.
Neuromodulation
For those with treatment-resistant depression:
- TMS (Transcranial Magnetic Stimulation): Uses magnetic pulses to stimulate nerve cells in the brain.
- ECT (Electroconvulsive Therapy): Often misunderstood, modern ECT is a highly controlled, safe, and effective last-line treatment for severe, life-threatening depression.
Lifestyle and Wellness
- Exercise: Regular aerobic exercise has been shown to be as effective as some antidepressants for mild to moderate depression.
- Sleep Hygiene: Since MDD and sleep are deeply linked, establishing a consistent circadian rhythm is a core component of recovery.
Frequently Asked Questions
Navigating the complexities of major depressive disorder medication often leads to common concerns regarding efficacy, safety, and long-term use. This section addresses the most frequent queries from patients and caregivers based on the 2026 clinical standards.
What is the most commonly prescribed medication for depression?
Currently, Sertraline (Zoloft) and Escitalopram (Lexapro) remain the most frequently prescribed antidepressants for major depressive disorder. Their popularity stems from a balanced profile of high efficacy and a relatively low risk of severe side effects compared to older drug classes.
How long does it take for antidepressants to work?
While the biochemical effects on neurotransmitters begin almost immediately, the clinical relief of mood symptoms typically takes 4 to 8 weeks to reach full effect. However, some patients notice improvements in sleep and energy levels within the first 1 to 2 weeks. For those requiring urgent relief, rapid-acting options like Esketamine (Spravato) or the new Auvelity can show results within days.
Can I stop my medication once I feel better?
No. Most guidelines recommend continuing medication for at least 6 to 9 months after you begin feeling better to prevent a relapse. Stopping too soon is one of the leading causes of MDD recurrence. If you have experienced multiple depressive episodes, your doctor may suggest long-term maintenance therapy for several years.
What should I do if my first antidepressant doesn’t work?
About two-thirds of patients do not achieve full remission with the first medication they try. If a 6-to-8-week trial at a therapeutic dose fails, your doctor may suggest:
- Switching: Moving to a different class (e.g., from an SSRI like Zoloft to an SNRI like Cymbalta).
- Augmentation: Adding a second medication, such as a low-dose antipsychotic (Abilify, Rexulti) or a mood stabilizer (Lithium), to “boost” the original antidepressant.
- Combination Therapy: Adding evidence-based psychotherapy (CBT or IPT) to the pharmacological regimen.
Are there long-term side effects of taking antidepressants?
While generally safe for long-term use, some patients may experience persistent side effects such as:
- Weight Gain: Certain medications (like Mirtazapine or Paxil) may affect metabolism over several years.
- Sexual Dysfunction: This is a common reason for discontinuation; clinicians often manage this by adding Bupropion or switching to a “serotonin-sparing” drug.
- Emotional Blunting: Some users report feeling “numb” or less able to feel intense joy or sadness, which often requires a dose adjustment.
Is it safe to drink alcohol while taking antidepressants?
Generally, it is advised to avoid or strictly limit alcohol. Alcohol is a central nervous system depressant that can counteract the benefits of your medication. Furthermore, mixing the two can increase drowsiness, impair coordination, and, in the case of MAOIs, cause dangerously high blood pressure.
Conclusion
Major Depressive Disorder is a formidable clinical challenge, yet it remains one of the most treatable mental health conditions. As we have explored throughout this 4,000-word guide, the key to success lies in a personalized, evidence-based treatment for depression. Whether through the “gold standard” SSRIs or the innovative rapid-acting glutamatergic agents of 2026, the primary goal of major depressive disorder medication is to restore the biological foundation of the brain, enabling the patient to engage fully in life and therapy.
The Power of Integrated Care
While medication acts on the neurochemistry, it is most effective when paired with the best therapeutic interventions for depression, such as Cognitive Behavioral Therapy. This “dual approach” ensures that both the biological symptoms and the psychological patterns are addressed simultaneously.
Looking Forward
For those who have not found relief in traditional pills, the horizon of psychiatry has never been brighter. With the rise of esketamine monotherapy, at-home neuromodulation devices, and the refinement of TMS protocols, “treatment-resistant” no longer means “untreatable.”
Recovery from MDD is not a straight line, but with the right major depressive disorder medication and a dedicated support team, the “fog” of depression can be lifted. If you or a loved one is struggling, the most critical step is the first one: seeking a professional evaluation to find the best antidepressant for depression tailored specifically to your biology and needs.
Authoritative References
1. National Institute of Mental Health (NIMH) – Mental Health Medications
2. U.S. Food and Drug Administration (FDA) – Depression Medicines Guide
3. American Psychological Association (APA) –Clinical Practice Guidelines
4. Mayo Clinic – Antidepressants: Selecting the Right One
5. PubMed Central (PMC) – Systematic Review of Approved Psychiatric Medications
Subscribe to Our Newsletter
Get mental health tips, updates, and resources delivered to your inbox.











