How a Person With Bipolar Thinks: Inside the Mind, Relationships, and Daily Life
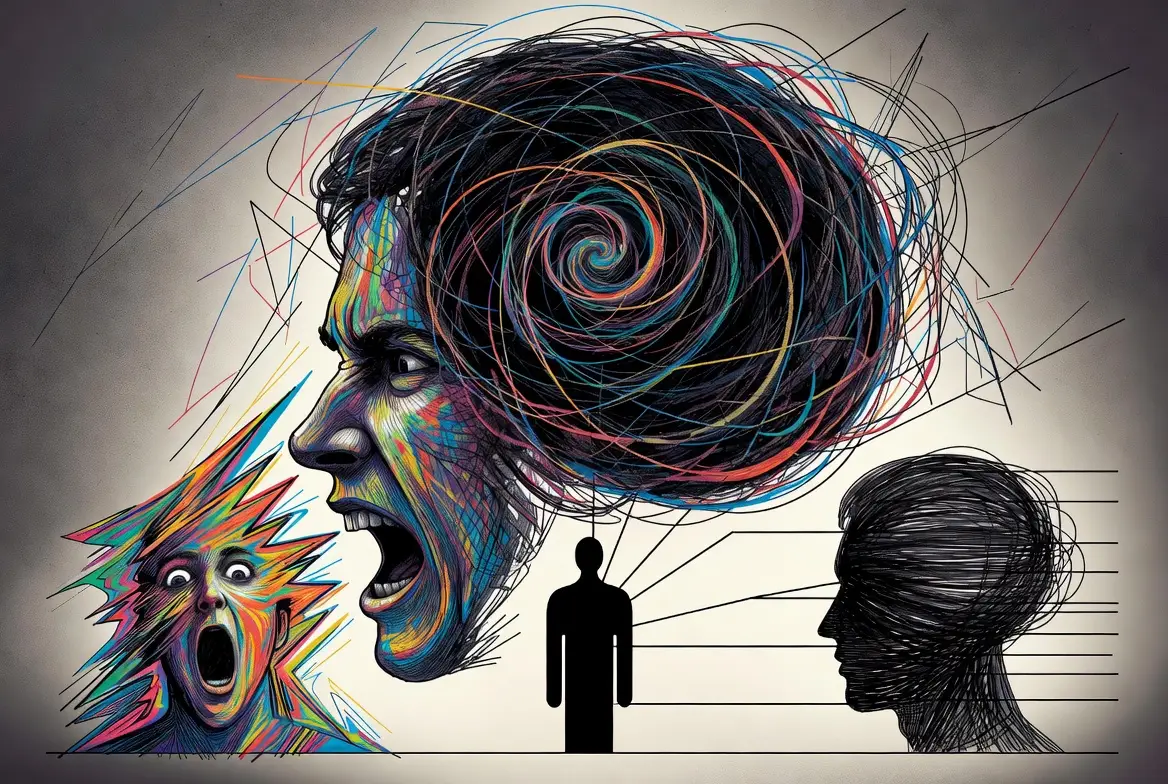
Understanding the internal architecture of a person’s mind is a complex task, but when that mind is shaped by bipolar disorder, the landscape becomes a shifting terrain of intensity, creativity, and profound challenge. To ask how a person with bipolar disorder thinks is to dive into a world where thoughts are not just ideas, but are deeply colored by the physiological state of the brain’s mood-regulation system.
For partners, family members, and those living with the diagnosis, understanding these thought patterns is the key to empathy, stability, and successful relationships. This comprehensive guide explores the cognitive processes of bipolar disorder, moving beyond the surface-level symptoms to reveal the “how” and “why” behind the behaviors.
What Does “How a Person With Bipolar Thinks” Really Mean?
When we discuss how a person with bipolar disorder thinks, it is vital to establish a foundational truth: bipolar disorder affects the tempo and filter of thought, not the person’s core intelligence, morality, or personality.
Thought Patterns vs. Character
A common misconception is that a person “is” their disorder. In reality, bipolar disorder acts like a seasonal climate for the mind. Just as a physical landscape looks different in a blizzard than it does in a heatwave, a person’s thoughts about how a person with bipolar disorder thinks are heavily influenced by their current “mood state.”
Mood-State-Dependent Thinking
Psychiatrists refer to this as mood-congruent processing. This means that when the brain is in a specific state—mania, depression, or euthymia (stability)—it selectively filters information to match that state.
- In Mania: The brain prioritizes rewards, possibilities, and connections.
- In Depression: The brain prioritizes risks, losses, and failures.
- In Euthymia, the brain can balance these inputs with a higher degree of objectivity.
Understanding this helps demystify why a person may seem like a “different person” depending on the month. They are the same individual, but they are processing reality through a significantly different neurological lens.
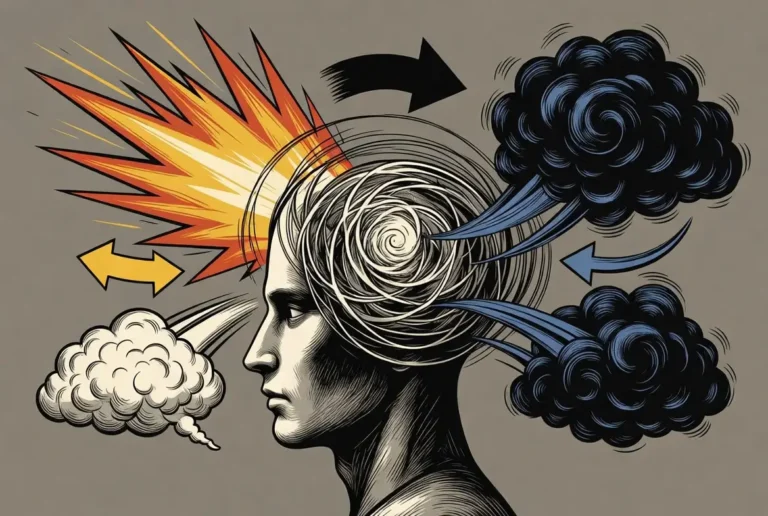
How a Person With Bipolar Thinks During Mania or Hypomania
The hallmark of mania or hypomania is a state of “hyper-drive.” In this state, the prefrontal cortex—the part of the brain responsible for impulse control and logical weighing of consequences—often takes a backseat to the limbic system, which drives emotion and reward-seeking.
Racing Thoughts and Rapid Idea Switching
One of the most frequent descriptions of racing thoughts, how a person with bipolar think,s is a “thought pressure.” Ideas don’t just arrive; they collide. This is clinically known as “flight of ideas.”
- The Experience: It feels like having twenty browser tabs open, all playing different videos at once.
- The Result: To an observer, this looks like bipolar confusion. The person may jump from a plan to start a business to a deep philosophical realization about a childhood memory within a single sentence.
Inflated Confidence vs. Insight Loss
During mania, the “internal critic” is silenced. This leads to an inflated sense of self-regard. Thoughts shift from “I could try this” to “I am destined for this.” Because the brain is bathed in dopamine, every idea feels like an “Eureka!” moment. Unfortunately, this often comes at the cost of insight, meaning the person may not realize their thoughts have become unrealistic until the episode begins to fade.
Black-and-White Thinking
Manic thinking tends to be polarized. Situations are either “the best thing ever” or “an obstacle that must be destroyed.” This lack of nuance makes it difficult for a person in mania to negotiate or see the “grey areas” of life, which often leads to the interpersonal friction that families experience.
How a Person With Bipolar Depression Thinks
On the opposite end of the spectrum, how a person with bipolar depression thinks is characterized by a profound “slowing down” of the cognitive machinery. This is often more than just sadness; it is a metabolic and neurological shutdown.
Slowed Thinking and Cognitive Fog
In a depressive state, the brain experiences “psychomotor retardation.”
- The Experience: It feels like thinking through molasses. Recalling a simple word or making a basic decision (like what to eat) can feel as exhausting as solving a complex equation.
- The Result: This leads to profound frustration, which further fuels the depressive cycle.
Hopelessness and Rumination
While mania looks forward with unrealistic optimism, bipolar depression looks backward with agonizing regret. The mind enters a loop of rumination, where every past mistake is replayed on a loop.
- Cognitive Distortions: The mind convinces the person of “facts” that aren’t true: “Everyone hates me,” “I am a burden,” or “It will never get better.” Understanding someone with bipolar depression requires realizing that these aren’t just “pessimistic moods”—they are perceived as objective, inescapable truths.
How a Person With Bipolar II Thinks
Bipolar II is often misunderstood as “Bipolar Lite,” but the internal experience is uniquely challenging. How a person with bipolar 2 thinks is defined by the absence of full mania and the presence of deep, chronic depression and “hypomania.”
Hypomania vs. Full Mania
In Bipolar II, hypomania often feels like a “super-version” of oneself. The thoughts are fast and productive, but they don’t usually break entirely from reality. Because of this, the person may feel they are just “doing great” until the inevitable crash into depression.
Higher Self-Awareness and Shame
Individuals with Bipolar II often maintain a higher degree of insight during their highs than those with Bipolar I. While this sounds positive, it often leads to a heavy burden of shame. They are aware enough to see their behavior changing, but may feel powerless to stop the shifting tide, leading to a thought pattern of constant self-monitoring and anxiety.
Bipolar Delusions, Obsessional Thinking, and Reality Testing
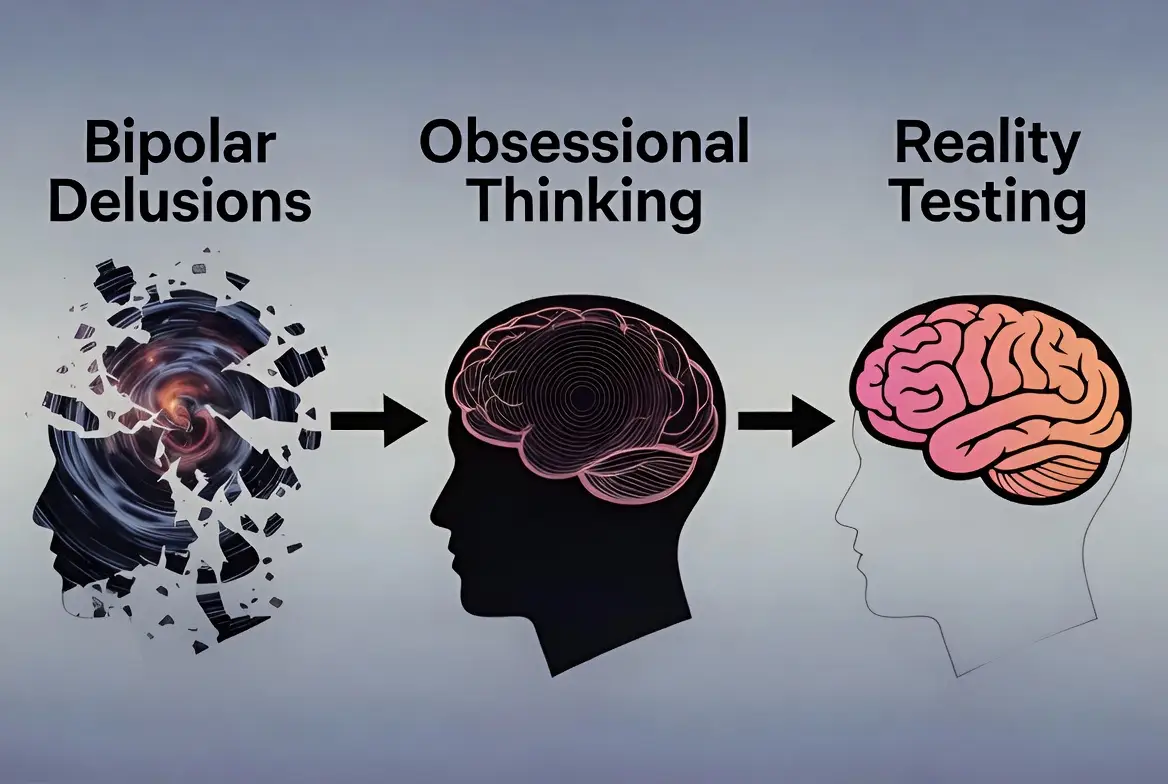
In severe cases, bipolar thinking moves beyond “moody” and into the realm of bipolar delusions and obsessional thinking. This is most common in Bipolar I during acute manic or depressive episodes.
Understanding Delusions
A delusion is a fixed, false belief that is resistant to reason.
- Grandiose Delusions: Believing one has special powers, is a secret celebrity, or has been chosen for a divine mission.
- Persecutory Delusions: Believing that the “racing thoughts” are actually being broadcast or that the government is monitoring them.
Obsessional Thinking
This differs from OCD. In bipolar disorder, obsessions are often “mood-locked.” In mania, one might become obsessed with a specific project or person (limerence). In depression, one might become obsessed with a physical ailment or a perceived moral failing.
Are People With Bipolar Self-Aware?
The question of whether bipolar people are self-aware is one of the most frustrating for loved ones. The answer is: It depends on the day.
Fluctuating Insight (Anosognosia)
During stable periods, most people with bipolar disorder are highly self-aware and proactive about their health. However, as a mood episode intensifies, a phenomenon called anosognosia can occur. This is a physiological “lack of insight” where the brain’s ability to self-monitor is disabled.
- The “Manic Blind Spot”: The person isn’t “lying” when they say they are fine; their brain is literally unable to perceive the dysfunction.
- The Role of Mood Tracking: This is why therapy and mood-tracking apps are vital. They allow the person to use objective data to “override” their subjective (and currently impaired) self-awareness.
Are People With Bipolar Disorder Dangerous?
It is essential to address the stigma: Are people with bipolar disorder dangerous? Statistically, the answer is a resounding no.
Evidence vs. Stigma
Research consistently shows that people with bipolar disorder are far more likely to be the victims of violence than the perpetrators. The primary risk of physical harm in bipolar disorder is actually directed inward, through self-harm or suicide during depressive or mixed episodes.
Symptoms vs. Character
While a person in a manic state may be loud, erratic, or argumentative, this rarely translates into planned violence. Most “dangerous” perceptions come from the unpredictability of the disorder, not malicious intent. Separating the symptoms (agitation) from the character (the person) is the first step in reducing the harmful stigma that prevents people from seeking help.
Bipolar Behaviors in Adults
When examining bipolar behaviors in adults, it is helpful to see them as the outward manifestation of the internal thought patterns we just discussed. Behavior is the “output” of the brain’s current “mood software.”
Examples of Manic and Hypomanic Behavior
- Pressured Speech: Because the thoughts are racing, the person talks faster than usual. They may be difficult to interrupt or jump between topics without a clear bridge.
- Impulsive Spending: The “reward center” of the brain is hyper-responsive. The thought “I need a new car” becomes an irresistible command because the brain isn’t calculating the long-term debt.
- Decreased Need for Sleep: A person may feel fully rested after only two or three hours of sleep. This is different from insomnia; they don’t want to sleep because they feel too energized.
- Hyper-Sociability: They may call friends at 3:00 AM or strike up intense conversations with strangers, driven by a feeling of universal connection.
Examples of Depressive Behavior
- Social Withdrawal: The actions of a bipolar person in depression often involve “ghosting” friends and family. It isn’t a lack of love, but a lack of the energy required to mask their pain.
- Executive Dysfunction: Simple tasks like opening mail or doing laundry become insurmountable. This is often mistaken for “laziness,” but it is actually a cognitive breakdown.
- Avolition: A total lack of drive to perform goal-directed activities.
How a Person With Bipolar TDisorder Hinks in Relationships
Relationships are perhaps the most impacted area of life. How a person with bipolar disorder thinks in relationships is often a tug-of-war between a deep desire for stability and the disruptive nature of mood swings.
Attachment Sensitivity and Fear of Abandonment
Many people with bipolar disorder carry a subconscious fear that their “episodes” will eventually drive people away. This can manifest in two ways:
- Hyper-Attunement: They become incredibly sensitive to a partner’s tone or facial expression, fearing it signals a breakup (often linked to past trauma or rejection).
- Pushing Away: During a mood shift, they may preemptively “break up” with a partner to avoid being the one who is left.
Emotional Intensity
In a relationship, a bipolar person’s “volume” is often turned up. Joy is euphoric; anger is explosive; sadness is soul-crushing. This intensity can be exhilarating during the “highs” but exhausting for a partner during the “lows.”
How Does a Bipolar Person Love?
A common question from partners is: How does a bipolar person love? The answer is: deeply, but sometimes inconsistently in expression.
Deep Emotional Bonding
Because many people with bipolar disorder experience such a wide range of human emotions, they often possess a profound capacity for empathy and emotional depth. When stable, they are often exceptionally attentive and creative partners.
Mood-Dependent Expression
It is important to understand that while their love is consistent, their ability to express it changes.
- During Mania: Love may be expressed through grand gestures, expensive gifts, or intense physical passion.
- During Depression: Love might look like simply allowing you to sit in the room with them while they are unable to speak. It is a quieter, more vulnerable form of love.
Can You Trust a Bipolar Person?
The question: Can you trust a bipolar person? often stems from the unpredictability of manic behavior.
Trust vs. Symptoms
Trust should be built on the person’s character, while the disorder is managed as a health condition.
- The Manic Exception: If a person makes a promise while manic, their brain may literally be unable to keep it once they crash. This isn’t a “lie” in the traditional sense; it’s a symptom of impaired reality testing.
- Accountability: Healthy trust is built when the person with bipolar disorder takes accountability for their treatment (medication, therapy) and creates “safety contracts” with their partner for when episodes occur.
Bipolar Manipulation Tactics: Myth vs. Reality
One of the most stigmatized search terms is Bipolar manipulation tactics. It is vital to differentiate between intentional malice and the impulsivity of the disorder.
Manipulation vs. Impulsivity
What looks like manipulation is often a desperate attempt to regulate an internal storm.
- Impulsive Requests: A person might “guilt” a partner into giving them money during mania. This isn’t a planned “tactic”; it’s an urgent, dopamine-driven impulse.
- Defensiveness: When a partner points out manic behavior, the person might become defensive. This is usually anosognosia (lack of insight) rather than a calculated “gaslighting” attempt.
True manipulation involves a cold, calculated intent to harm or control. Most bipolar behaviors are “hot,” impulsive reactions to overwhelming emotions.
Arguing With a Bipolar Person
Arguing with a bipolar person during an active episode is often counterproductive because their “logic centers” are temporarily offline.
What Escalates Conflict
- Logic-Checking: Trying to “prove” they are wrong during mania often leads to increased agitation.
- Shaming: Using their disorder as a weapon (e.g., “Are you off your meds?”) usually shuts down communication.
What Helps De-escalation
- The “Wait and See” Approach: If an argument starts during a high or low, try to postpone the “heavy” discussion until they are more stable.
- Validation: You can validate their feelings (“I see that you are very angry”) without agreeing with their delusions or unrealistic plans.
What Happens When You Ignore a Bipolar Person?
What happens when you ignore a bipolar person can vary depending on their current state, but it is generally a high-risk strategy.
- During Mania: They may feel deeply rejected or “persecuted,” leading to more erratic behavior to get your attention.
- During Depression: Being ignored can confirm their internal narrative that they are “worthless” or “better off gone,” increasing the risk of self-harm.
Healthy Disengagement: Instead of “ignoring,” use “boundary-setting.” For example: “I love you, but I cannot have this conversation while you are shouting. I am going to the other room for an hour, and we can try again then.”
How to Live With Someone With Bipolar
Learning how to live with someone with bipolar disorder is a journey of patience and structure.
Boundaries and Support
- Don’t Enable, But Do Support: You can support their recovery by helping with routines, but you shouldn’t “cover” for them by lying to their boss or paying off manic debts.
- Crisis Planning: When the person is stable (euthymic), sit down and write a plan. Who do we call if you stop sleeping? Which hospital do you prefer? This takes the guesswork out of a crisis.
Understanding Someone With Bipolar Disorder
To truly achieve understanding of a bipolar person, one must look past the “noise” of the symptoms to the person underneath. This requires a shift in perspective: seeing bipolar disorder not as a character flaw, but as a chronic physiological condition, much like diabetes or asthma.
Empathy Without Excusing Harm
Understanding someone with bipolar disorder involves a delicate balance. It means acknowledging that their brain is misfiring, while still maintaining personal boundaries.
- The “Biological” View: You recognize that their irritability in a mixed state is a result of neurochemical agitation.
- The “Behavioral” View: You still require them to participate in treatment and offer apologies once they are stable. Empathy provides the context, but accountability provides the path to a long-term relationship.
What Triggers Bipolar Episodes?
Thinking patterns don’t shift at random. Usually, there is a catalyst. Knowing what triggers bipolar episodes is the best defense against a major relapse.
- Sleep Disruption: This is the most potent trigger. Even one night of missed sleep can “flip the switch” into hypomania for a vulnerable brain.
- High-Stress Life Events: Major changes—even positive ones like a wedding or a promotion—can trigger an episode due to the sheer amount of cognitive processing required.
- Substance Use: Alcohol and drugs (including excessive caffeine) interfere with the brain’s rhythm and can render medications ineffective.
- Seasonal Changes: Many people with bipolar disorder experience a “seasonal pattern,” often dipping into depression in the winter and rising toward mania as the days get longer in the spring.
How Do People With Bipolar Live Day to Day?
A common question is: How do people with bipolar ldisorder ive? Can they hold jobs? Can they be parents?
The Reality of High-Functioning Bipolar
Many individuals with bipolar disorder are “high-functioning.” They work as doctors, lawyers, artists, and teachers. Their daily life is built on extreme discipline.
- Routine as Medicine: Successful management often involves a rigid schedule—going to bed at the same time every night, avoiding alcohol, and taking medication with the same consistency as one would take insulin.
- The “Internal Thermostat”: They spend a significant amount of mental energy “checking” their own thoughts. “Am I happy because I’m having a good day, or am I happy because I’m becoming manic?”
Famous People and How a Person With Bipolar Thinks
Looking at famous people, how a person with bipolar disorder thinks can offer a glimpse into the creative power that sometimes accompanies the disorder. While it brings suffering, the “unfiltered” thinking of hypomania can also lead to extraordinary innovation.
- Carrie Fisher: The late actress and author spoke eloquently about the “fast” thinking of her mania and the “slow” pain of her depression, becoming a beacon of self-aware advocacy.
- Kanye West: His public struggles have highlighted the challenges of bipolar delusions and the difficulty of maintaining treatment in the public eye.
- Stephen Fry: His documentaries have provided a deep dive into the “oscillating” mind, showing how a person can be brilliant and articulate while still struggling with a profound internal darkness.
Frequently Asked Questions (FAQ)
How does a bipolar person think differently?
A bipolar person’s brain filters reality through their current mood state. In mania, the brain ignores risks and amplifies rewards. In depression, the brain amplifies pain and ignores possibilities.
Are bipolar people manipulative?
Usually, no. Behaviors that look like manipulation are typically impulsive reactions to overwhelming emotions or a lack of insight (anosognosia) during an active episode.
Can bipolar people maintain long-term relationships?
Yes. With consistent treatment, open communication, and clear boundaries, people with bipolar disorder can and do have successful, decades-long marriages and partnerships.
Do bipolar people know when they’re unwell?
Not always. During a severe episode, the brain’s “self-monitoring” system can shut down. This is why having a trusted support system to provide “reality checks” is essential.
Is bipolar thinking permanent?
No. Thinking patterns are “state-dependent.” When a person is stable (euthymic), their thinking is typically no different from that of someone without the disorder.
Conclusion
To understand how a person with bipolar disorder thinks, we must replace fear with curiosity. Bipolar disorder is a complex, often grueling condition, but it is not a sentence to a life of chaos. By recognizing the racing thoughts of mania and the heavy silence of depression as biological events rather than character flaws, we can bridge the gap between “us” and “them.”
Whether you are the one living with the diagnosis or the one standing beside them, remember that the goal isn’t to “fix” the mind, but to support the person. With the right combination of medication, therapy, and a deeply informed support system, the bipolar mind can find its way back to a reality that is stable, meaningful, and full of love.
Authoritative References
1. National Institute of Mental Health (NIMH) – Bipolar Disorder
2. Harvard Medical School (Harvard Health Publishing) – Bipolar Disorder
3. National Library of Medicine (NCBI) – Cognitive Impairment in Bipolar Disorder
4. Depression and Bipolar Support Alliance (DBSA) – Relationships and Bipolar
5. The Lancet – Bipolar Disorder (Clinical Review)
Subscribe to Our Newsletter
Get mental health tips, updates, and resources delivered to your inbox.