Borderline Personality Disorder in Children and Teens: A Guide for Parents
As a parent, few things are more distressing than watching your child struggle with emotions that seem too large for them to carry. When a child’s mood swings are not just frequent but explosive, or when their fear of being left alone leads to frantic behavior, parents often find themselves searching for answers. This search frequently leads to a specific, often misunderstood clinical term: borderline personality disorder.
While borderline personality disorder in children is a topic fraught with controversy and clinical debate, it is a subject of growing importance in the field of developmental psychology. Historically, clinicians were hesitant to discuss personality disorders in anyone under the age of 18, believing that personality is too fluid during youth to warrant such a heavy label. However, modern research suggests that the precursors to this condition often appear long before adulthood.
What Is Borderline Personality Disorder?
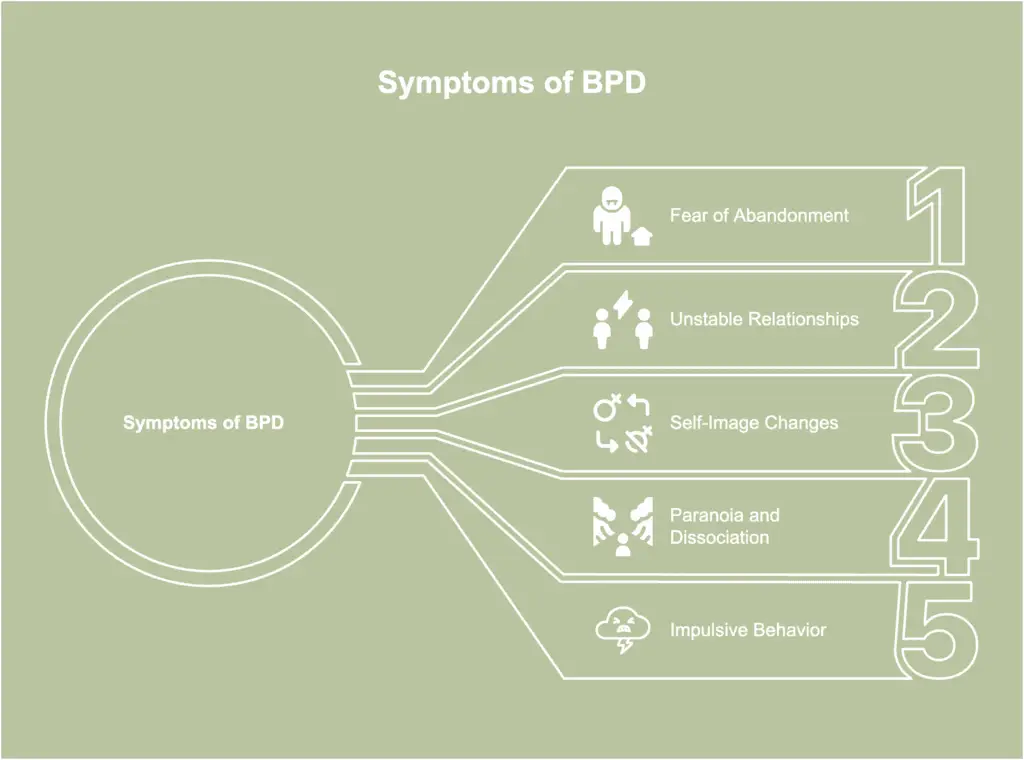
To understand borderline personality disorder, it helps to view it not as a “broken” personality, but as a profound struggle with emotional regulation. Clinically, BPD is a mental health condition characterized by a pervasive pattern of instability in affects (emotions), self-image, and interpersonal relationships, along with marked impulsivity.
Core Features of BPD
For a parent, these clinical terms translate into everyday struggles. The “instability of affects” means your child may experience emotional “flooding,” where they are so overwhelmed by a feeling that they cannot access logic or reason. The “identity disturbance” may manifest as a child who seems to change their entire personality based on who they are with.
The Developmental Perspective
The DSM-5 (the diagnostic manual used by professionals) outlines nine criteria for BPD, including chronic feelings of emptiness, intense anger, and frantic efforts to avoid abandonment.
However, in the borderline personality disorder early years, these symptoms often look different than they do in adults. Clinicians today view BPD as a developmental disorder—meaning it is a way of processing the world that begins in childhood and solidifies over time.
Recognizing “early traits” is not about labeling a child as “borderline” forever; it is about identifying that their emotional “alarm system” is hypersensitive so they can receive the right help early on.
At What Age Does Borderline Personality Disorder Develop?
One of the most common points of confusion is the timeline of the disorder. Parents often ask: At what age does borderline personality disorder develop?
The Adolescent Onset
Traditionally, the “typical” age for a formal diagnosis is late adolescence (17–19) or early adulthood. This is because the brain’s prefrontal cortex—the part responsible for regulating the emotional centers—undergoes massive changes during these years.
It is clinically inappropriate to give a full diagnosis of BPD to a very young child. For example, discussing a 5 year old borderline personality disorder diagnosis is almost never done in professional settings. At five, a child’s brain is naturally impulsive and ego-centric; what looks like a BPD trait is often just a developmental milestone or a reaction to environmental stress.
The 12-Year-Old Marker
As children enter puberty, the picture changes. We see an uptick in parents concerned about bpd in 12 year olds. This is the age where the intersection of hormonal shifts and social pressure can cause underlying emotional vulnerabilities to surface.
While a 12-year-old might not receive a formal diagnosis, they may be identified as having “borderline traits.” This distinction is important: it acknowledges the severity of the behavior while leaving room for the child’s personality to continue evolving.
Early Signs of BPD in Children
While we do not diagnose young children with personality disorders, researchers have identified certain early signs of bpd in children that may indicate a higher risk for developing the disorder later. It is vital to frame these as vulnerabilities rather than a fixed destiny.
Patterns to Observe
- Extreme Emotional Reactions: A child who stays upset for hours over a minor disappointment, or whose “baseline” is much higher than their peers.
- Fear of Abandonment: Not just typical “stranger danger,” but a frantic, panicked reaction if a parent leaves the room or if a friend chooses to play with someone else.
- Black-and-White Thinking: A child who views people as “all good” one minute and “all bad” the next (splitting).
- Intense Attachment Patterns: Signs of bpd in childhood often involve “velcro” attachments—becoming intensely, almost obsessively attached to a teacher or a peer, followed by a total withdrawal if they feel slighted.
- High Impulsivity: Behavior that goes beyond typical “naughtiness,” involving a total lack of “brakes” when the child is emotional.
These borderline personality disorder in children often overlap with other conditions. If your child shows these traits, it is a signal to look closer at their emotional regulation skills, not to assume a permanent diagnosis.
What Does Borderline Personality Look Like in a Child?
When parents ask, “What does borderline personality look like in a child?” they are usually looking for a way to describe the “vibe” of their home life. In a child with these traits, the environment often feels “high-voltage.”
Comparison Table: Behavior vs. Clinical Traits
| Typical Childhood Behavior | BPD-Like Emotional Patterns | Trauma-Related Behavior |
| Tantrums that end when the child gets what they want or is distracted. | Meltdowns that escalate regardless of the outcome; “emotional flooding.” | Hyper-vigilance or “shutting down” as a survival reflex. |
| Preferring one parent over another (phases). | Intense “splitting”—seeing one parent as a hero and the other as a villain. | Fear-based attachment or avoidance of caregivers. |
| Forgetting rules due to being distracted or excited. | Breaking rules as a way to “test” if the parent will still love them or stay. | Impulsivity driven by a “fight or flight” nervous system. |
It is essential to note that borderline personality disorder in children symptoms can be nearly identical to symptoms of ADHD, Autism Spectrum Disorder (ASD), or Complex PTSD. A child who has experienced attachment disruption or trauma may mirror BPD traits almost perfectly because their brain is stuck in survival mode.
Signs of BPD in Teens: How Adolescence Changes the Picture
As a child transitions into their teenage years, the borderline personality disorder in teens presentation becomes much clearer and often more high-stakes. This is the period where “traits” may coalesce into a clinical picture.
What are signs of BPD in teens?
In adolescence, the symptoms often migrate from the home into the social and academic spheres.
- Relationship Instability: A teen may have a “new best friend” every month, with each relationship ending in a dramatic “burnout.”
- Identity Disturbance: This goes beyond typical teenage “finding yourself.” The teen may frequently change their name, their sexual orientation, their style, and their core values in a desperate attempt to find a “mask” that fits.
- Self-Harm vs. Emotional Regulation: In bpd in 12 year olds and older, self-harm (like cutting) is often used as a way to “feel something” or to ground themselves when they feel emotionally overwhelmed.
- Impulsive Risk-Taking: This might include reckless spending, substance use, or risky sexual encounters, often done in a moment of emotional pain to “numb out.”
Adolescence is a “pressure cooker” for BPD traits because the need for peer acceptance is at an all-time high, while the fear of rejection is at its most potent.
Petulant Borderline Personality Disorder
When exploring the various manifestations of this condition, clinicians often refer to the Millon model of BPD subtypes. One specific pattern that parents frequently identify is Petulant Borderline Personality Disorder.
While these subtypes are descriptive rather than official diagnostic categories, they help explain why BPD doesn’t look the same in every child.
What are the symptoms of petulant borderline personality disorder?
In a child or teen, the “petulant” pattern is characterized by extreme irritability, cynicism, and a passive-aggressive style of relating to others.
- The “Unloved” Narrative: The child often feels deeply unappreciated and unloved, even in the face of evidence to the contrary.
- Stubbornness and Defiance: They may be incredibly difficult to please, often “testing” parents by acting out to see if the caregiver will eventually reach a breaking point.
- Moodiness and Sulking: Instead of the explosive rage seen in other types, the petulant subtype often involves long periods of “the silent treatment” or brooding dissatisfaction.
Parents often recognize this subtype first because it creates a home environment where everyone feels they are “failing” the child, despite their best efforts to provide love and stability.
The “3 C’s” of Borderline Personality Disorder
If you are a parent of a child struggling with these traits, the weight of guilt can be paralyzing. You may spend your nights replaying every mistake you ever made, wondering, “Is it my fault my daughter has borderline personality disorder?” To combat this, mental health advocates and clinicians emphasize the 3 C’s of BPD:
- I didn’t Cause it: BPD is a complex biosocial condition. While environment plays a role, children are often born with a biological vulnerability—a “highly sensitive” nervous system. You did not give them this temperament.
- I can’t Control it: You cannot force your child to regulate their emotions. No amount of “perfect” parenting can fix a clinical emotional processing disorder.
- I can’t Cure it: While you are an essential part of the support system, the “cure” involves professional therapy and the child’s own development of coping skills over time.
Internalizing these principles is the first step in moving from a place of “shame” to a place of “effective support.”
Parenting and BPD: How the Disorder Affects Family Dynamics
How does borderline personality disorder affect parenting? The reality is that it often turns the household upside down. Parenting a child with borderline personality disorder is not like typical parenting; it is more akin to being a first responder in a constant state of high alert.
Common Family Challenges
- Walking on Eggshells: Family members may stop speaking their truth or expressing their own needs to avoid “triggering” the child’s next meltdown.
- Emotional Burnout: Caregivers often experience “compassion fatigue,” leading to a sense of numbness or resentment that causes further guilt.
- Co-Parenting Conflict: BPD traits often “split” parents. One parent may be seen as the “all-good” protector, while the other is the “all-bad” disciplinarian, leading to severe marital strain.
- Sibling Impact: Siblings may feel neglected or “quiet” to compensate for the high-needs child, sometimes leading to their own mental health struggles or a “parentification” role where they try to fix the family.
Being the Child of Someone with Borderline Personality Disorder
While much of the focus is on children exhibiting traits, we must also address the intergenerational cycle: being the child of someone with borderline personality disorder.
If a caregiver has untreated BPD, the child often grows up in an “invalidating environment.” Because the parent’s emotions are so large and unpredictable, the child’s own emotional needs are often pushed aside. This can lead to attachment trauma, where the child learns that their feelings are “wrong” or “too much.” Breaking this cycle is the primary goal of family-based interventions, ensuring that the next generation has the emotional tools the previous one may have lacked.
Does My Child Have BPD? Screening, Tests, and Quizzes

In moments of desperation, many parents turn to the internet, searching for a borderline personality disorder in children test or a “Does my child have BPD?” quiz.
The Truth About Online Screening
It is essential to understand that no online quiz can diagnose a child with BPD. These tools are often designed for adults or are based on “pop psychology” that pathologizes normal teenage behavior.
- Professional Assessment: A real assessment involves clinical interviews, developmental history, and observation by a child psychologist or psychiatrist.
- The Goal of Screening: A clinician may use screening tools to identify “traits” or “vulnerabilities,” but the purpose is to guide treatment, not to stamp a permanent label on a developing child.
Child Personality Disorders: What Else Could It Be?
Because personality is still forming, symptoms that look like BPD are often actually symptoms of other conditions. When reviewing a child personality disorders list, it is crucial to consider “differential diagnoses.”
- ADHD: Both involve impulsivity and emotional outbursts, but ADHD is primarily about attention and “brakes,” whereas BPD is about attachment and abandonment.
- Autism Spectrum Disorder (ASD): “Meltdowns” in ASD are often due to sensory overload, while BPD meltdowns are triggered by perceived rejection.
- DMDD (Disruptive Mood Dysregulation Disorder): This is a relatively new diagnosis for children who have chronic, severe irritability and frequent temper outbursts, often used in place of a BPD or Bipolar label in kids.
- PTSD / Complex Trauma: Children who have experienced trauma often show identical symptoms to BPD because their nervous system is permanently stuck in “fight or flight.”
How Many Children Have BPD? Prevalence & Statistics
When we look at how many children have BPD, the data is often difficult to pin down. This is largely because clinicians prefer to use terms like “emerging personality patterns” or “dysregulation” rather than the formal BPD label in youth.
Understanding the Numbers
In the adult population, the prevalence of BPD is estimated to be around 1.6% to 5.9%. However, in adolescent clinical settings (teens seeking mental health help), that number jumps significantly, with some studies suggesting up to 11% to 22% of outpatient teens meet the criteria.
The reason for the discrepancy is twofold:
- Under-diagnosis: Many clinicians still fear that a BPD label will “stigma-mark” a child for life, leading them to use “Adjustment Disorder” or “Depression” as placeholder diagnoses.
- Over-diagnosis: During the height of puberty, almost every teen exhibits some BPD-like traits (impulsivity, moodiness). Distinguishing between a permanent personality structure and a temporary developmental phase requires expert longitudinal observation.
BPD in Kids Treatment: What Actually Helps
The most important message for parents is that BPD traits are no longer considered “untreatable.” In fact, because children’s brains have high neuroplasticity, early intervention can lead to a complete remission of symptoms before the child reaches adulthood.
Evidence-Based Approaches
1. DBT-C (Dialectical Behavior Therapy for Children): This is a modified version of DBT specifically for pre-adolescents. It focuses on teaching “Super-Parenting” skills alongside the child’s skills. Parents learn how to become “emotional coaches” who validate their child’s feelings while maintaining firm boundaries.
2. DBT-A (Adolescents): Designed for teens, this includes a “Walking the Middle Path” module, which specifically addresses the “push-pull” conflict between teens and parents.
3. Trauma-Informed Care: If the BPD traits are rooted in early childhood trauma or attachment disruption, therapies like EMDR or Attachment-Based Family Therapy (ABFT) are essential to heal the underlying nervous system dysregulation.
4. Medication: There is no medication specifically for BPD. However, doctors may prescribe low-dose mood stabilizers or SSRIs to treat “comorbid” conditions like severe anxiety or depression, which can make BPD symptoms harder to manage.
How to Explain Borderline Personality Disorder to a Child
If your child or teen is receiving treatment for BPD traits, they may feel “broken” or “weird.” How to explain borderline personality disorder to a child requires removing the clinical jargon and focusing on the experience of their nervous system.
A Script for Parents:
“You know how some people have a really sensitive nose and can smell things others can’t? You have a really sensitive ’emotional heart.’ You feel happy things way bigger than most people, but you also feel sad or angry things way bigger, too. Sometimes it feels like an emotional storm. Our job is to help you learn how to be a professional sailor so you can navigate those waves without the boat tipping over.”
Focusing on the “Superpower” of their sensitivity—their empathy and creativity—helps them build an identity that isn’t entirely defined by their struggles.
Frequently Asked Questions
What are signs of BPD in teens?
The primary signs include a frantic fear of being left alone, “splitting” (viewing people as heroes or villains), impulsive self-harm, a lack of a clear sense of self, and intense, short-lived “emotional storms.”
At what age does borderline personality disorder develop?
While traits can be seen as early as 8 to 10, the disorder typically crystallizes in late adolescence (16–19). Formal diagnosis is rarely given before age 12.
Does my child have BPD quiz—are they accurate?
No. These quizzes cannot account for the child’s developmental age, trauma history, or other conditions like ADHD. They should only be used as a prompt to seek professional help.
Is it my fault my child has BPD?
No. BPD is a biosocial condition. It results from a child’s innate temperament interacting with their environment. You did not choose their temperament.
Can BPD go away with treatment?
Yes. BPD has a very high “remission” rate. With therapies like DBT, most young people learn to regulate their emotions so effectively that they no longer meet the criteria for the disorder as adults.
Conclusion
The journey of understanding borderline personality disorder in children and teens is not about finding a label to stick on a child; it is about finding a language for their pain.
If your child is showing signs of extreme emotional instability, the most important thing you can do is seek support that focuses on emotional regulation rather than a lifelong diagnosis. Traits are not destiny. With early intervention, a “highly sensitive” child can grow into an adult with high emotional intelligence, profound empathy, and a stable, fulfilling life. You are your child’s best advocate, and by seeking out evidence-based information, you have already taken the first step toward their recovery.
Authoritative References
1. Child Mind Institute – Borderline Personality Disorder in Teenagers
2. National Education Alliance for Borderline Personality Disorder (NEA.BPD)
3. McLean Hospital – Adolescent Dialectical Behavior Therapy (DBT) Program
4. American Academy of Child & Adolescent Psychiatry (AACAP) –Practice Parameters
5. National Institute of Mental Health (NIMH) –Borderline Personality Disorder
Subscribe to Our Newsletter
Get mental health tips, updates, and resources delivered to your inbox.






